
A rare case of self-inflicted foreign body in the urethra of a pediatric patient which was successfully managed with urethrotomy converted into urethrostomy: a case report
Highlight box
Key findings
• A fascinating and exceptionally uncommon instance of a self-inflicted foreign object found in the urethra of a pediatric patient.
• No previous literature has reported identifying 10 needles in the urethra.
• The aim of the treatment is to extract the foreign body with minimal complications as possible.
• If there are concerns regarding stricture formation, performing a urethrostomy will reduce morbidity.
What is known and what is new?
• There is a plethora of documentation detailing instances of self-inflicted foreign bodies in various bodily openings among pediatric patients. Extensive discussion has taken place regarding the management of diverse foreign objects in different anatomical sites. Nonetheless, occurrences of foreign bodies, such as needles in the urethra, continues to be exceedingly uncommon.
• This manuscript emphasizes the significance of early diagnosis, deliberations of selecting appropriate radiological assessments, and the array of surgical treatment options.
What is the implication, and what should change now?
• Foreign bodies in the urethra among pediatric patients continue to be uncommon. Often, diagnosing them upfront poses a challenge due to the vague medical history associated with such cases. The most effective strategy for removal of foreign bodies is directly influenced by their location, size, shape, surgical proficiency and available equipment.
• Management should be individualized according to case scenario.
Introduction
Foreign body insertion into the urethra is rather uncommon within the pediatric age group and it has been rarely reported in literatures (1). It is a rare urological emergency with potentially dire consequences. Diagnosis can be arduous unless the insertion is confessed upfront. The presentation is usually delayed due to the feeling of shame and embarrassment. Here, we report a rare case in which a 5-year-old boy had self-inflicted 10 needles into the urethra. This case warrants a discussion as there is no available literature that has reported of 10 needles in a urethra. The clinical presentation and treatment strategy are discussed in order to enhance disease awareness and facilitate early diagnosis. We present this article in accordance with the CARE reporting checklist (available at https://jphe.amegroups.com/article/view/10.21037/jphe-24-31/rc).
Case presentation
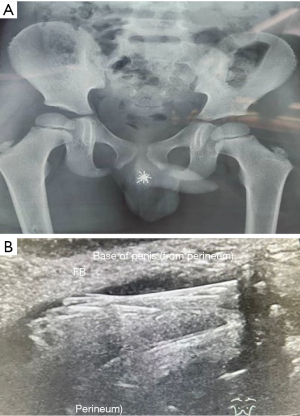
A 5-year-old boy with no significant past medical history was referred to our department with the chief complaint of bloody discharge from the urethral meatus for 2 days which was associated with burning sensation over the penis and a limping gait. He had no formal history of mental or psychiatric disorder at that point. Detailed questioning revealed that he had self-inserted multiple needles into his urethra, he could not describe the exact size of the needle. Physical examination of the patient revealed normal findings with no signs of trauma at the external genitalia. White cell counts, haemoglobin, platelet count and renal profile were within normal limit. There were also no signs of bacterial infection on urinalysis as well. Anterior posterior pelvic radiograph revealed a clump of fine linear radio-opaque shadow in the region of urethra (Figure 1A). An ultrasound of the penis and scrotum was done to gauge the number of needles and its location, the findings of the ultrasound revealed that there were at least 7 needles which are orientated longitudinally within the urethra and corpus spongiosum, there was no adjacent collection or free fluid seen (Figure 1B). The needles measured approximately 3.7 cm each. The sharp needle tip is directed towards the penile tip while the head is towards the base. The tip of the needle is located approximately 4.6 cm from the tip of the penile head. A computer tomography (CT) scan was not done as there was no suspicion of the needles being migrated or caused a perforation. CT scan also carries undesirable risk associated with procedural sedation and radiation exposure. Cystoscopic examination confirmed that there were a total of 10 needles. The ball end of the needles was located at the posterior urethra, near the veru montanum. Transurethral route of cystoscopic retrieval was attempted but unsuccessful, and abandoned as there were too many needles, which logically carries additional risk of urethral injury. A urethrotomy was performed via perineal incision (Figure 2A) and 10 needles were delivered out safely (Figure 2B). Likelihood of injury to the epithelial lining of the urethra from cystoscopic instrumentation was a major concern as there could be a possible stricture if primary closure was performed. With given expertise and limited experiences of dealing with this rare case, performing a primary closure in a damaged/edematous tissue would not have a favourable outcome. Henceforth urethrotomy was converted into urethrostomy (Figure 3).

While the primary aim of treatment remains by the extraction of foreign body, it is essential to factor in potential short-term and long-term complications, including but not limited to strictures, incontinence and urethral diverticula. These complications vary depending on factors such as the depth of initial insertion, frequency of foreign body insertion and the method required for extraction. Post operatively, he recovered well and prior to discharge a psychiatric evaluation was performed and he was later diagnosed with autism spectrum disorder. He remained well throughout his follow up which was at the first and third month in which later the urethrostomy was closed as the patient established normal voiding without any complications.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s parents for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
The act of self-insertion of foreign body into the urethra is an uncommon occurrence and it is often associated to a condition known as polyembolokoilamania. This disorder entails patient inserting foreign objects into bodily orifices for a multitude of reasons, ranging from psychopathological motives to urological procedures, self-stimulation, enhancement of erections, seeking attention, or simply out of curiosity (2).
Polyembolokoilamania has been documented in medical literature for an extended period, yet comprehensive analysis and examination of this behavior remains sparse to date. This disorder is almost always accompanied by a background psychiatric condition (3). The diagnosis of urethral polyembolokoilamania should be relatively straightforward, but patients are usually not forthright due to the stigma associated with this behavior, making the diagnosis challenging. Owing to the wide array of sizes, shapes, compositions, and placement of urogenital tract foreign bodies, the clinical presentation they elicit are diverse. Bladder foreign bodies typically manifest with spasmodic abdominal pain, hematuria, a feeling of incomplete urination, and urinary interruption. Conversely, urethral foreign bodies commonly present with urgency, penile pain, dysuria, hematuria and difficult in urinating (4). When evaluating a suspected urethral foreign body, it is essential to meticulously review the patient’s medical history, symptoms, clinical examination findings, and imaging studies in a thorough and integrated approach. As there are lack of literature-based guidelines with regards to common practice, the treatment strategy for this current case is guided by accurate localization and configuration of self-inserted needles with plain radiograph and ultrasound assessment. For non-radiopaque foreign bodies, plain radiography offers a straight forward means of visualization, enabling direct assessment of their shape and dimensions. With a specificity up to 91%, plain radiography is typically adequate for identifying both metallic and non-radiopaque foreign bodies, facilitating their localization and characterization. Ultrasound assessment has become increasing popular and reliable with an overall 81% sensitivity of detecting urogenital foreign body. It is known to be safe, radiation free, non-invasive, cost effective and comfortable for pediatric patients, making it the preferred diagnostic tool (5). A CT scan offers superior soft tissue imaging capabilities and enhanced diagnostic utility in cases where ultrasound or conventional radiography fail to ascertain the presence or displacement of a foreign body (6). In a nutshell plain radiograph typically gives a general idea of the foreign body, however, ultrasonography or computerized tomography may be required for accurate diagnosis. CT is usually indicated when the urethral foreign body is suspected for having migrated to adjacent organs (7). As mentioned, in this current case, the radiological examination of choice was plain radiograph followed by ultrasound assessment as the patient was hemodynamically stable and there were no signs or symptoms pointing towards the migration of foreign body. Efforts in addressing retained foreign body should focus on thorough removal, striving to minimize any associated complications to the greatest extent possible. Visualization via cystoscope provides a precise method of verification of urethral foreign body and in most instances, cystoscopic removal is deemed the optimal course of action (8). The success rate of transurethral route of cystoscopic retrieval is debatable as it depends on external factors such as the number of foreign bodies in the urethra, the position and configuration of the foreign body, surgeons experience in handling such case and availability of proper instruments. In pediatric population, extracting foreign bodies poses a formidable challenge, as the size of the pediatric urethra may hinder safe transurethral removal (9). In aforementioned case, the boy had 10 needles in his urethra for which transurethral route of cystoscopic retrieval was attempted. That was a comprehensive attempt, considering by the numbers and the position of the needles. Continued effort for cystoscopic retrieval was deemed with potential risk of urethral injury. Cystoscopic treatment is effective in some cases, in other cases, meanwhile, cystoscopic treatment fails because of the need to reduce urethral injury during transurethral removal of foreign body or due to the difficulty of grasping the foreign body, making open surgery become the choice of treatment (9). In our case, we opted for a safer and reliable approach via urethrotomy. We did not embark on primary closure of the urethra as there was plenty of manipulation via instrumentation which can cause epithelial injury and may predispose the patient to stricture and available surgeon experience at that point. Thus, precautions were taken and urethrostomy was done. Alternative surgical method would have been to embark on a primary closure with a longer duration of catheterization post operatively. Increasing the duration of catheter retention may be beneficial in lowering the probability of developing post operative urethral stricture. Approach and managements are tailored according to case base scenario which aims to give the best outcome for the patient, taking into consideration of available expertise at the point of time.
Conclusions
Foreign bodies in urethra amongst the pediatric age group remain rare. Most of the time, it remains as a challenge in making up front diagnosis because of the ambiguous medical history. Holistic approach towards these kinds of patients would be beneficial. To ascertain the exact location, size, configuration and number of foreign bodies, one can use plain radiograph, ultrasound assessment or CT scan. Each of these modalities has their own benefit and limitation. Surgical treatment should be considered early after confirmation of foreign body. The primary objective of surgical intervention is to successfully extract the foreign body while mitigating the occurrence of complications to the greatest extent possible. The best approach for removal of foreign bodies depends directly on their location, size, configuration, surgical expertise and available equipment. Available surgical options are usually between cystoscopic removal or open surgical removal of foreign body. Management should be individualized according to case scenario. There is a debate as to whether patients who have inserted foreign bodies into their urethra requires a necessary psychiatric assessment. It may be worthwhile considering the high incidence of mental illness in these patients. The paramount reason to exclude mental illness is to prevent or avoid a case of recurrence. Empowering parents through education to enhance awareness of potential risk is also an efficacious preventive strategy.
Patients perspective
The patient expressed immense gratitude for surviving the incident and acknowledged the dedication and care provided by the medical team.
Acknowledgments
The authors thank all the efforts provided by the paediatrics surgery team from Hospital Tunku Azizah, Kuala Lumpur, Malaysia.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://jphe.amegroups.com/article/view/10.21037/jphe-24-31/rc
Peer Review File: Available at https://jphe.amegroups.com/article/view/10.21037/jphe-24-31/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jphe.amegroups.com/article/view/10.21037/jphe-24-31/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s parents for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ceran C, Uguralp S. Self-inflicted urethrovesical foreign bodies in children. Case Rep Urol 2012;2012:134358. [Crossref] [PubMed]
- Vahidi S, Karami H, Gholizadeh H. Case report: Removal of a big sewing needle from a boy's urethra from the skin for the first time. Urol Case Rep 2021;38:101662. [Crossref] [PubMed]
- Layek AK, Majumder U, Baidya I. Polyembolokoilamania with obsessive compulsive and related disorders: A case series. Indian J Psychiatry 2023;65:484-6. [Crossref] [PubMed]
- Tao C, Peng B, Mao C, et al. Diagnosis and treatment strategies for pediatric urogenital tract foreign bodies: A retrospective study. Am J Emerg Med 2024;79:12-8. [Crossref] [PubMed]
- Yang X, Sun L, Ye J, et al. Ultrasonography in Detection of Vaginal Foreign Bodies in Girls: A Retrospective Study. J Pediatr Adolesc Gynecol 2017;30:620-5. [Crossref] [PubMed]
- Zheng L, Cho YC, Shin JH, et al. Percutaneous antegrade removal of foreign bodies in the urinary tract: a 20-year, single-center experience. Acta Radiol 2021;62:1097-103. [Crossref] [PubMed]
- John J, Kesner K. Urethral polyembolokoilamania: not a bread-and-butter issue. Ther Adv Urol 2021;13:17562872211022866. [Crossref] [PubMed]
- Untan I, Ersekerci E. A sewing needle as a urethral foreign body: A case report and literature review. Niger J Clin Pract 2023;26:1588-90. [Crossref] [PubMed]
- Kuang T, Cai W, Qian W, et al. Foreign bodies in children's lower urinary tract: A case series and literature review. Front Pediatr 2022;10:1095993. [Crossref] [PubMed]
Cite this article as: Praemanathan H, Arasappan M, Fernandez JEG, Abdullah MY. A rare case of self-inflicted foreign body in the urethra of a pediatric patient which was successfully managed with urethrotomy converted into urethrostomy: a case report. J Public Health Emerg 2024;8:19.



