The relationship of the mean glandular dose with compressed breast thickness in mammography
Introduction
Breast cancer is the most frequent cancer and cause for cancer-induced deaths in women in Europe (1,2). Early detection through mammographic screening systematically is the most effective and feasible method to substantially lower current breast cancer mortality and reduce the burden of this disease in the population (3). Mammography is the most widely used method in breast diagnostic procedure. However, there is a small risk of radiation induced carcinogenesis associated with the mammographic procedure and this made the estimation of the absorbed dose to the gland tissue of the breast an important part of the quality control of the examination. Mean glandular dose (MGD) is usually used to estimate the breast dose in several protocols such as European Commission protocol and IAEA protocol. MGD is difficult to measure directly and can be estimated by multiplying the incident air kerma with a series of conversion factors. Monte-Carlo method is introduced in several studies such as Dance to calculate the conversion factors which was tabulated as result of these studies (4,5).
The aim of this manuscript is to observe the relationship of the MGD level with CBT in the diagnostic mammographic procedure and discuss the mechanisms of the relationship.
Methods
Mammography equipment
Eighteen hospitals in five cities were picked in China. Seventeen are public hospitals and one is private hospital.
One mammography system was selected in each sample hospital and in these 18 equipments, 10 of them are DR and 7 of them are CR system and 1 of them are SFR system. The details of the equipments were displayed in the Table 1.
Table 1
| Model | Manufacturer | Number | Type |
|---|---|---|---|
| Senographe DS | GE | 1 | DR |
| Senographe 2000D | GE | 3 | DR |
| Senographe | GE | 1 | CR |
| Affinity | Hologic | 1 | CR |
| Alpha RT | GE | 1 | CR |
| Selenia | Hologic | 3 | DR |
| Gitto | Gitto | 1 | DR |
| Nuance | Planmed | 1 | DR |
| Sophie Classic | Planmed | 1 | CR |
| Mammomat 1000 | Siemens | 2 | CR |
| Mammomat Nova | Siemens | 1 | DR |
| MAMMOMAT3000 NOVA | Siemens | 1 | CR |
| Flat-BYM | METALTRONICA | 1 | SFR |
Patient data
A total of 360 radiographic mammography exposures were picked from the exposures in these sample hospitals to take part in the study. Forms containing exposure parameters (include voltage, tube load) and patient information were filled by the technicians who perform these examinations in sample hospitals. The CBT (compressed breast thickness) was provided by the scale of the mammography equipment and was confirmed with a ruler. Data of 20 different exposures [10 for craniocaudal (CC) and 10 for mediolateral oblique (MLO)] who had a mammography examination were gathered in each hospital at the time period of Sep 2012 to Mar 2013.
Measurement of MGD
The MGD for each acquired image was calculated according to Dance’s study (4,5), using the formula MGD = K∙g∙c∙s [1]
K is the incident air kerma (K) at the upper surface of the breast, measured without backscatter. And g, c and s are Monte Carlo calculated conversion factors. The factors g is the incident air kerma (K) to MGD factor for a breast of 50% glandularity. The c-factor corrects for any difference in breast composition from 50% glandularity. The s factor is used to correct differences arising from the use of X-ray spectra generated by anode target/filter combinations other than Mo/Mo. All the source of these three factors is from the Dance’s study by Monte-Carlo method (5).
K and half value layer (HVL) data were obtained with a QA radio dosimeter (model: Barracuda; RTI Corporation, Sweden) after the investigation forms were collected from the sample hospitals. The mammography equipment were operated to make an exposure according to the parameters (tube voltage; tube output, target/filter combination) recorded in the form and the incident air Kerma (K) were measured by the QA radio dosimeter. The QA radio-dosimeter was calibrated in the traceable Secondary Standard Dosimetry Laboratory at the Shanghai Institute of Measurement and Testing Technology (SIMT). The measurements were performed in the time period from Jan, 2013 to Mar, 2013. Two sets of 99.9% purity aluminum filter were used for HVL measurements. Measurements were corrected according to the inverse-square law for each individual breast thickness.
Statistical analysis
Linear regression was performed by SPSS, version 19.0. Correlation analyses were performed by tow-tailed Spearmen test to verify the significant of the functions fitted by linear regression.
Result
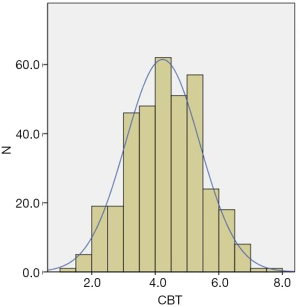
In order to observe the relationship of the MGD (unit: mGy) and the exposure parameters with the CBT, information of the 360 exposures and the CBT were analyzed. The CBT of the patient population ranged from 13 to 75 mm. Mean thickness was 42 mm with standard deviation of 12 mm. The distribution of the CBT fitted the nominal distribution with kurtosis of −0.327 and skewness of 0.004. The Figure 1 showed the distribution of the CBT.
The distribution of the CBT is shown in Figure 1.
The relationship of the MGD with the CBT
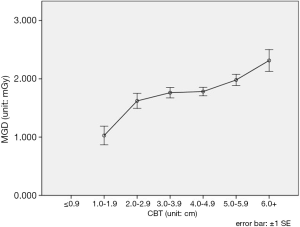
MGDs of the mammographic procedure were calculated by using the eq. [1]. Figure 2 showed the MGD level of the different CBT group and it showed a current that the MGD may increase with CBT. Linear regression was used to fit a function (y=0.151·x+0.195). However, the correlation between the two variables was not so well fitted (R2=0.043, P<0.01).
The relationship of the MGD composition factors and the CBT
In order to observe the trend of the MGD composition factors (K, g, c) with CBT, K (incident air kerma), g-factor and c-factors against the CBT was showed in Figure 3A, B and C.
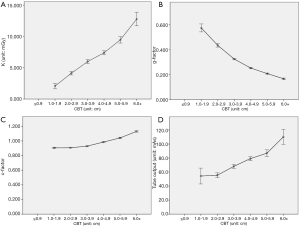
The Figure 3A, B and C suggested that K and c-factor have a positive correlation and g-factor has a negative relation with CBT. The result of the correlation analysis was showed in the Table 2.
Table 2
| Factors | K | g-factor | c-factor |
|---|---|---|---|
| Correlation | 0.547** | −0.902** | 0.936** |
| P value | 0.001 | 0.001 | 0.001 |
**, correlation is significant at the 0.01 level (2-tailed). CBT, compressed breast thickness.
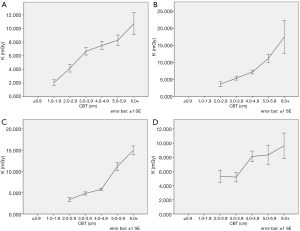
The relation of the MGD with the CBT with different brand
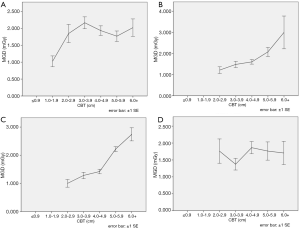
In order to minimize the uncertainties originate from the technology of the different manufacturers, the data were categorized to four groups (GE, Hologic, Planmed and Siemens). Two equipments from other two manufacturers were deleted in this part of results. Figure 4A,B,C,D showed the MGD level of different CBT group in these four brands mammography equipments.
Discussion
For the reason of the relative high sensitivity of the glandular tissue in woman breast, many studies focused on the breast dosimetry in mammographic procedure and these studied showed that the MGD could be influenced by many factors (6,7). Part of these factors came from the equipments such as tube voltage (unit: kV), tube output (unit: mAs) and HVL while part of these factors came from the patient. The most important factor from patient is CBT which is known as CBT.
Some previous studies showed that the CBT could have a significant effect on MGD in mammography (8,9). The positive correlation of MGD with CBT showed in present study was similar to some previous studies (8,10-12). However, the function fitted by linear regression could not fit so well (R2=0.043, P<0.01) and that is similar with the result of a previous study in Turkey (13). The curve displayed in Figure 2 showed a platform at the range between 30 and 50 mm. This result was similar with CNT mode result in a previous research by Chen who had studied the relation of MGD with CBT by three kinds of AEC modes in a Senographe 2000DS FFDM system and Chen believed there might be other factors playing important roles in this process (14).
From the present study it can be concluded that the relation between MGD and CBT is complicated. Among the four compositions in the right side of the eq. [1], three factors named K, g and c could be affected by CBT.
The relationship of the CBT with incident air kerma (K)
Incident air kerma (K) is the most majority influential factor of all factors in the eq. [1]. K showed a positive correlation with CBT from the Figure 3A. The mechanism is that a bigger CBT which means a thicker woman breast would increase the density judgment made by the equipment in AEC mode and it would increase the tube output (unit: mAs). Consequently, this would increase the incident air kerma (K) of the mammography procedure. The linear relation of tube output with CBT displayed in Figure 4D showed that the K and tube output (unit: mAs) varied the same pattern as CBT increase and the relation of K with tube output showed in Figure 5 showed K had a strong correlation with tube output (unit: mAs).
The relationship of the CBT with coefficient factors (g-factors and c-factors) in Dance’s model
In Dance’s model, g-factors and c-factors had a relationship with CBT in different direction and this represent different mechanisms that CBT would affect MGD level.
In the study of Dance, g-factor was defined as coefficient from K to MGD for a breast of 50% glandularity. A model breast was defined in the Monte-Carlo program of the Dance’s study. The factor was estimated as the ratio of the energy absorbed in the glandular tissues to the product of the incident air kerma (K) and the mass of the glandular tissue present in the central region of the breast.
On the circumstance of the K is fixed, although a thicker breast which means a bigger CBT could increase the energy deposit in the breast tissue but the increased mass of glandular tissue could decreased the absorbed dose (unit: Gy). This is the reason why the g-factor decreases as CBT increases.
The c-factors affected by CBT in the opposite direction with the g-factors do. The function of the c-factors is to correct the MGD difference originate from composition of the breast which is called glandularity of the breast. Several study on glandularity showed that the thicker breast tend to have a less glandularity (5,15). So a thicker compressed woman breast which means a bigger CBT would make the c-factors change towards the same direction as the smaller glandularity that means a decrease of the breast density and that could increase the MGD. On the other hand, the glandularity of the woman breast could be affected by the age (16-18). This is why the Dance gave two tables of the c-factors for different age group.
A series of simple linear regression were made to compare the effect degree of the three factors in the right side of the eq. [1] and the results of the linear regressions in the Table 3 indicated that K is the most majority influential factors of the three.
Table 3
| MGD composition factors | Coefficient | Constant | Function | R2 | P value |
|---|---|---|---|---|---|
| K | 2.050 | −1.194 | y=2.050·x−1.194 | 0.310 | 0.001 |
| g-factor | −0.072 | 0.584 | y=−0.072·x+0.584 | 0.765 | 0.001 |
| c-factor | 0.054 | 0.756 | y=0.054·x+0.756 | 0.806 | 0.001 |
Note: correlation is significant at the 0.01 level (2-tailed). MGD, mean glandular dose.
Table 4 summarized the mechanisms of how the CBT influence the MGD.
Table 4
| MGD composition factors | Mechanisms |
|---|---|
| K | CBT↑→optical density↑→tube output↑→K↑→MGD↑ |
| g-factor | CBT↑→mass of the breast↑→energy deposit per mass unit↓=MGD↓ |
| c-factor | CBT↑→glandularity↓→density of the breast↓→mass↓→energy deposit per mass unit↑=MGD↑ |
CBT, compressed breast thickness; MGD, mean glandular dose.
The relation of the MGD with the CBT with different brand
In a solo equipment study the MGD may be affected by the CBT through the mechanism above, however a new situation appeared in a multiple equipments study that the MGD may be affected by the parameter select technology in AEC mode of different manufacturers. Figure 4 showed the relationship of MGD versus CBT in different brand of equipment in present study. The figures showed that the MGD in Hologic group and Planmed group had a positive relation with CBT while the GE group and the Siemens group did not show a similar pattern. Figure 5 showed that the incident air kerma (K) against CBT in different brand groups and all these four curves showed a trend of increase with CBT. The results of Figures 4 and 5 indicated that although the K would increase with CBT increases, however, with the effect of coefficient factors the output of MGD may display a different current. The reason of this situation is the different patterns of the K versus CBT and these patterns may have different causes such as technology of the manufacturers, different AEC modes in some brands which were reported in Chen’s study (14).
Additionally, image type (CR, DR or SFR) of the equipment could also effected the MGD level in this kind of situation which was reported in a previous analysis (7,19).
Character and limitation
The character of the present study was to focus on the trend of the MGD on population perspective. Information of mammography exposures from 18 mammography set were analyzed, unlike some previous research which study the trend of the MGD on one or several equipments. It could bring us the basis of a quick method to evaluate the glandular dose to the population.
Four brands of equipments was categorized and analyzed to minimize the uncertainties from the manufacturers’ technology.
Additionally, the limitation of the study is that the glandularity correction factor (c-factor) is based on studies from Europe and it may not be applicable to the Chinese female population.
Conclusions
In a range of 20 to 60 mm, MGD showed a positive correlation with CBT. The results of the present study indicated that CBT could influence the MGD through multiple pathways and these pathways represent different mechanisms.
Acknowledgments
This survey was supported by Jiangsu Provincial Center for Disease Prevention. We thank the co-operation of the staff at the mammography clinic of the Department of Radiology and the investigators of the Nanjing CDC, Xuzhou CDC, Suzhou CDC, Yancheng CDC and Zhenjiang CDC.
Funding: The study was supported by Jiangsu Province Health Development Project with Science and Education (No. ZX201109) and mainly supported by Jiangsu Province’s Outstanding Medical Academic Leader program (CXTDA2017029).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jphe.2017.03.10). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Boyle P, Ferlay J. Cancer incidence and mortality in Europe, 2004. Ann Oncol 2005;16:481-8. [Crossref] [PubMed]
- Ferlay J, Autier P, Boniol M, et al. Estimates of the cancer incidence and mortality in Europe in 2006. Ann Oncol 2007;18:581-92. [Crossref] [PubMed]
- Perry N, Broeders M, de Wolf C, et al. editors. European guidelines for quality assurance in breast cancer screening and diagnosis. Luxembourg: Office for Official Publications of the European Communities, 2006.
- Dance DR, Skinner CL, Young KC, et al. Additional factors for the estimation of mean glandular breast dose using the UK mammography dosimetry protocol. Phys Med Biol 2000;45:3225-40. [Crossref] [PubMed]
- Dance DR, Young KC, van Engen RE. Further factors for the estimation of mean glandular dose using the United Kingdom, European and IAEA breast dosimetry protocols. Phys Med Biol 2009;54:4361-72. [Crossref] [PubMed]
- Chevalier M, Morán P, Ten JI, et al. Patient dose in digital mammography. Med Phys 2004;31:2471-9. [Crossref] [PubMed]
- Du X, Wang J, Yang CY, et al. Investigation of mean glandular dose in diagnostic mammography in China. Biomed Environ Sci 2014;27:396-9. [PubMed]
- Jamal N, Ng KH, McLean D. A study of mean glandular dose during diagnostic mammography in Malaysia and some of the factors affecting it. Br J Radiol 2003;76:238-45. [Crossref] [PubMed]
- Jeukens CR, Lalji UC, Meijer E, et al. Radiation exposure of contrast-enhanced spectral mammography compared with full-field digital mammography. Invest Radiol 2014;49:659-65. [Crossref] [PubMed]
- Young KC, Burch A, Oduko JM. Radiation doses received in the UK Breast Screening Programme in 2001 and 2002. Br J Radiol 2005;78:207-18. [Crossref] [PubMed]
- Hendrick RE, Pisano ED, Averbukh A, et al. Comparison of acquisition parameters and breast dose in digital mammography and screen-film mammography in the American College of Radiology Imaging Network digital mammographic imaging screening trial. AJR Am J Roentgenol 2010;194:362-9. [Crossref] [PubMed]
- Baldelli P, McCullagh J, Phelan N, et al. Comprehensive dose survey of breast screening in Ireland. Radiat Prot Dosimetry 2011;145:52-60. [Crossref] [PubMed]
- Bor D, Tukel S, Olgar T, et al. Investigation of mean glandular dose versus compressed breast thickness relationship for mammography. Radiat Prot Dosimetry 2008;129:160-4. [Crossref] [PubMed]
- Chen B, Wang Y, Sun X, et al. Analysis of patient dose in full field digital mammography. Eur J Radiol 2012;81:868-72. [Crossref] [PubMed]
- Jamal N, Ng KH, McLean D, et al. Mammographic breast glandularity in Malaysian women: data derived from radiography. AJR Am J Roentgenol 2004;182:713-7. [Crossref] [PubMed]
- Beckett JR, Kotre CJ. Dosimetric implications of age related glandular changes in screening mammography. Phys Med Biol 2000;45:801-13. [Crossref] [PubMed]
- Boyd N, Martin L, Chavez S, et al. Breast-tissue composition and other risk factors for breast cancer in young women: a cross-sectional study. Lancet Oncol 2009;10:569-80. [Crossref] [PubMed]
- Mavi A, Cermik TF, Urhan M, et al. The effect of age, menopausal state, and breast density on (18)F-FDG uptake in normal glandular breast tissue. J Nucl Med 2010;51:347-52. [Crossref] [PubMed]
- Oduko JM, Young KC, Burch A. A Survey of Patient Doses from Digital Mammography Systems in the UK in 2007 to 2009. Heidelberg: Springer Berlin Heidelberg, 2010:365-70.
Cite this article as: Du X, Yu N, Zhang Y, Wang J. The relationship of the mean glandular dose with compressed breast thickness in mammography. J Public Health Emerg 2017;1:32.