
Worldwide epidemiology and trends of adenosine diphosphate (ADP) receptor inhibitors usage
Introduction
There is still debate on which antiplatelet agent should be added to, or substituted for, aspirin in the management of acute coronary syndrome, as well as in other cardiovascular diseases, such as cerebrovascular disease and peripheral artery occlusive disease (1-3). Although several of these drugs have been tested in many large trials, there are still concerns about their variable clinical efficacy and toxicity (4,5).
According to recent guidelines, the use of adjunctive antithrombotic therapy with adenosine diphosphate (ADP) receptor inhibitors [conventionally known as P2Y12 (receptor) inhibitors] in combination with aspirin is highly recommended for early treatment and for supporting reperfusion with primary percutaneous coronary intervention (PCI) in both patients with ST-elevation myocardial infarction (STEMI) and in those with non-ST elevation myocardial infarction (NSTEMI). In STEMI patients the American College of Cardiology Foundation/American Heart Association (ACCF/AHA) guidelines recommend a loading dose of one of the three P2Y12 inhibitors as early as possible or at time of PCI (clopidogrel 600 mg; prasugrel 60 mg; ticagrelor 180 mg), followed by a 1-year period of maintenance dosage (clopidogrel 75 mg daily; prasugrel 10 mg daily; ticagrelor 90 mg twice a day) (6). No major variations have been reported for this standard therapy in ensuing guidelines (7). The guidelines of the European Society of Cardiology (ESC) for patients with STEMI also recommend a loading dose of one of the three P2Y12 inhibitors as early as possible or at time of PCI (ticagrelor 180 mg; prasugrel 60 mg in clopidogrel-naive patients; clopidogrel 600 mg, eventually when prasugrel or ticagrelor are either not available or contraindicated). A maintenance dosage is then also recommended (ticagrelor 90 mg twice a day; prasugrel 10 mg daily; clopidogrel 75/150 mg daily) (8). The recommendations of both the AHA/ACC and the ESC guidelines for platelet inhibition in patients with NSTEMI are virtually identical (9,10).
The current armamentarium of P2Y12 receptor inhibitors entails three drugs classified under the name of thienopyridines (i.e., clopidogrel, prasugrel and ticlopidine) and two additional drugs classified under the generic definition of “nonthienopyridine” (cangrelor and ticagrelor) (11). Ticlopidine is the oldest P2Y12 inhibitor to be clinically used (12), and is now only prescribed in a minority of countries due to significant hematological toxicity (13). Clopidogrel is an inactive pro-drug needing oxidation by the hepatic cytochrome P450 (CYP) system to generate the active metabolite. An estimated 85% of the prodrug is hydrolysed by esterases into an inactive form, thus leaving only 15% of clopidogrel available for transformation into the active metabolite, which selectively and irreversibly inactivates platelet P2Y12 receptors and thus inhibits ADP-induced platelet aggregation (14). Unfortunately, a consistent number of patients have genetic variants of the CYP2C19 gene, which may contribute to reduce the concentration of the active metabolite during therapy (15). Albeit genetic testing and assessment of platelet function can identify patients at higher risk, the unsatisfactory predictability of platelet inhibition by clopidogrel has catalyzed the research for alternative drugs, eventually characterized by a more predictable effect. Prasugrel is a third-generation P2Y12 receptor inhibitor with a faster onset and a more profound inhibitory effect than clopidogrel, and is hence considered a suitable therapeutic alternative, since is effective for achieving high level platelet inhibition in a large majority of patients, including carriers of the CYP2C19*2 allele genotype (16). The other side of these advantages, however, is represented by the finding that in clinical studies severe bleeding complications were more common with prasugrel than with clopidogrel, due to an observed increase in both non-fatal and fatal bleeds (17). Ticagrelor is another reversible P2Y12 inhibitor, also exhibiting a more rapid and consistent onset of action compared with Clopidogrel, as well as a faster offset of action with more rapid recovery of platelet function (18). Finally, cangrelor is the only P2Y12 receptor inhibitor which needs parenteral administration.
Although the widespread availability of many P2Y12 inhibitors along with the strength of recommendations strongly supporting their use in patients with both STEMI and NSTEMI have contributed to enhance the popularity and prescription of these drugs around the world, no reliable information has recently been published about their worldwide use and popularity. Google Trends (Alphabet Inc. Mountain View, CA, United States) is a web instrument based on Google Search, displaying the frequency of how a specific term is searched in Google according to worldwide search volume (19). The final digital report is a graph displaying the relative frequency of a search term compared to the total number of searches during a certain period of time. The numbers are given in arbitrary scale (between 0 and 100), reflecting the Google search interest relative to the highest point on the chart. Accordingly, a number of 100 reflects the peak of popularity for the search term, 50 means that the search term had half popularity, whereas 0 means the search term was <1% as popular as the peak (19). This free web instrument is hence useful for gathering practical insights about the popularity of a given search term also in science and medicine. Notably, recent studies convincingly confirm that the number of web searches may provide a reliable approximation about the generic usage of many drugs, also allowing to identify significant variations in prescribing behaviors (20-22). Therefore, we planned an original study to collect information about the Web searches for P2Y12 inhibitors, as a first order approximation of their worldwide pharmaceutical use.
Methods
An electronic search was performed in Google Trends with the keywords “Clopidogrel” AND “Ticagrelor” AND “Ticlopidine” AND “Prasugrel” (i.e., the four most worldwide used receptor inhibitors), and using the search option “prescription drug”. The keyword “Cangrelor” ought to be initially omitted since this drug was not indexed by Google under the option “prescription drug” or simply “drug”, and the generic search also generated a negligible score (i.e., always <1). No language limit was used and the searches were performed from the first date available in Google Trends (i.e., January 1st, 2004) to present time (i.e., June 1st, 2017). The output of this electronic search was then displayed according to monthly volumes (i.e., the total score of each month) related to the highest peak of popularity (i.e., a Google Trends score of 100) throughout the entire search period. A sub-analysis was then carried out to identify more recent trends (i.e., in the past five years, between June 2012 and May 2017). The Google Trends scores were reported as monthly medians along with their interquartile range (IQR). The significance of difference of Google Trends scores during the search periods was assessed with Mann-Whitney U test and the trend over time (between months and the relative Google Trends score) was tested with Spearman’s correlation. The statistical analysis was performed using Analyse-it (Analyse-it Software Ltd, Leeds, UK). The study was carried out in accordance with the Declaration of Helsinki and under the terms of relevant local legislation.
Results
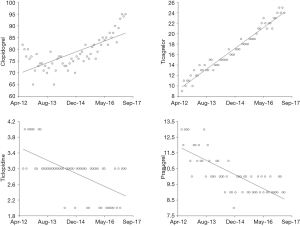
The results of the Google Trends score throughout the entire search period (i.e., from January 2004 to May 2017) is shown in Figure 1. The median monthly Google Trends score of clopidogrel was by far the highest among the four drugs (76; IQR, 71–80), nearly 8-fold higher than that of prasugrel (9; IQR, 3–11; P<0.001) and nearly 20-fold higher than that of ticlopidine (4; IQR, 3-5; P<0.001) and ticagrelor (3; IQR 0–14; P<0.001). The geographical distribution of the Google search volume is reported in Figure 2, which shows a wide heterogeneity for the popularity of these four drugs around the world. A rather different figure emerged when the Google Trends score was assessed before and after June 2012 (Table 1). In particular, between January 2004 and May 2012 the highest volume of monthly Google searches could be recorded for Clopidogrel, whereas the median score of the other three drugs was always <5. In the past five years the volume of monthly Google searches for clopidogrel further increased by approximately 4% (P<0.001), that of ticagrelor and prasugrel increased by nearly 17- and 2.5-fold (both P<0.001), whereas that of ticlopidine decreased by approximately 25% (P<0.001). The trends of Google searches for the four P2Y12 receptor inhibitors in the past 5 years (i.e., between June 2012 and May 2017) is shown in Figure 3. Interestingly, clopidogrel (r=0.68; 95% CI, 0.52 to 0.80; P<0.001) and especially ticagrelor (r=0.99; 95% CI, 0.98 to 0.99; P<0.001) exhibited a substantially increasing trend, whilst that of ticlopidine (r=−0.61; 95% CI, −0.75 to −0.42; P<0.001) and prasugrel (r=−0.75; 95% CI, −0.85 to −0.62; P<0.001) displayed a fairly significant opposite trend (Figure 3).
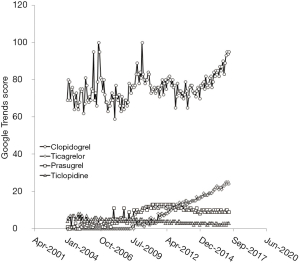
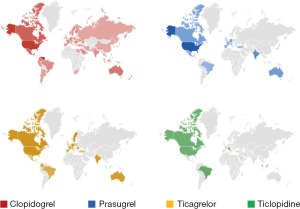
Table 1
| Drug | January 2004–May 2012 | June 2012–May 2017 | P |
|---|---|---|---|
| Clopidogrel | 74 (IQR, 69–79) | 77 (IQR, 74–82) | <0.001 |
| Ticagrelor | 0 (IQR, 0–2) | 17 (IQR, 14–21) | <0.001 |
| Ticlopidine | 4 (IQR, 4–5) | 3 (IQR, 3–3) | <0.001 |
| Prasugrel | 4 (IQR, 2–11) | 10 (IQR, 9–11) | <0.001 |
Discussion
The use of antiplatelet agents in combination with aspirin (i.e., the so-called “dual antiplatelet therapy”) for immediate management of patients with arterial thrombotic diseases is now advocated by the most followed guidelines around the world (6-10). After many years of monopoly of ticlopidine, clopidogrel first, and relatively new molecules like prasugrel and ticagrelor afterward, have been introduced and are now widely used in many countries, especially in US and Europe (23). The choice of the P2Y12 inhibitor is often subjective, since the practice guidelines do not provide clear recommendations or unequivocal data of clinical superiority, major efficacy or greater safety of one drug compared to the others (6-10). This complex scenario has hence prompted us to perform a first order approximation of their worldwide pharmaceutical use based on Google Trends data, a freely available web instrument which was proven quite reliable for investigating drug usage and variations of prescribing behaviors (22).
The first important aspect emerged from our analysis is that the popularity of ticlopidine (i.e., the first P2Y12 receptor inhibitors to be introduced in the market, nearly 40 years ago) (Table 2) has consistently decreased over time, especially in the past 5 years (Figure 3). Quite interestingly, the Google search volumes for this drug in the past 5 years could only be identified in US, Italy and Brazil, so confirming a widespread perception that its era may have come to an end (23). This aspect is strongly supported by clinical evidence showing that this Ticlopidine has been associated with a number of important side effects, especially with reduction of white blood cell and development of thrombotic thrombocytopenic purpura (TTP), which have led to discontinuation of ticlopidine in the US since the 2015 (24).
Table 2
| Drug | FDA | EMA | Worldwide sales (year 2015)* |
|---|---|---|---|
| Clopidogrel | November, 1997 | July, 2008 | 2,141 million US$ |
| Ticagrelor | July, 2011 | December, 2010 | 619 million US$ |
| Ticlopidine | October, 1991 | March, 1978# | Not currently available |
| Prasugrel | July, 2007 | February, 2009 | 773 million US$ |
*, not including the sales of generic drugs; #, only in a number of European countries. FDA, US Food and Drug Administration; EMA, European Medicines Agency.
Clopidogrel has been the second P2Y12 receptor inhibitor to be approved for clinical use, nearly 20 years ago in the US and nearly 10 years ago in Europe, respectively (Table 2). Since then, the popularity of this drug has constantly increased (Table 1), as also mirrored by the highest volume of sales among all the P2Y12 receptor inhibitors. Not only clopidogrel has been the most popular drug searched in Google in the past 5 years, but also the Google Trends score shows an increasing trend, especially in the past 3 years (Figure 3). Notably, the volume of Google Searches seems quite homogenous worldwide, with a peak of popularity in the US (Figure 2).
Prasugrel is another thienopyridine which has been first approved for use in patients with acute coronary syndrome nearly 10 years ago (Table 2). Despite an early raise of popularity soon after its introduction, the Google search volumes of this drug have dramatically decreased during the past 5 years (Figure 3). Most of these come from the US (Figure 2), with the Google Trend score virtually limited to this country in the past 12 months (data not shown). The gradual decline in popularity of this drug, especially in Europe, is possibly linked to the fact that the ESC guidelines advice against administering Prasugrel in patients in whom the coronary anatomy is unknown (6-10).
Ticagrelor is the most recent of these drugs, since it has been approved by the US Food and Drug Administration (FDA) in July 2011 and by the European Medicines Agency (EMA) in December 2010 (Table 2). This clearly explains the growing interest for this compound, which is conceivably mirrored by an increasing number of prescriptions especially in North America, Western Europe, Australia, India and Brazil (Figure 2). Among all P2Y12 receptor inhibitors, the Google Trends score of Ticagrelor has displayed the sharpest (nearly linear; r=0.99) increase during the past 5 years (Figure 3), which is probably attributable to the many advantages of this drug. Unlike clopidogrel and prasugrel, ticagrelor is not a prodrug necessitating activation and has a reversible effect on P2Y12 receptor blockade. Moreover, this drug has large applicability throughout the entire spectrum of acute coronary syndrome, managed both medically and invasively, with constant efficacy among multiple subgroups of patients (11). According to our data, it seems hence conceivable that the popularity of this drug will predictably increase in the following years. As regards cangrelor, it is quite surprising that the volume of Google search for this drug was virtually inexistent compared to the other of P2Y12 receptor inhibitors. This may be due to the fact that this drug was only recently approved (June 2015 by both the FDA and by the EMA) and is only administered with intravenous infusion (25), so that the popularity in terms of Web searches may be still in its infancy.
Conclusions
The results of our analysis of Google Trends score of P2Y12 receptor inhibitors attest that the popularity of ticlopidine and prasugrel has apparently declined in recent times, that of clopidogrel has remained quite constant over more than a decade, whereas that of ticagrelor seems constantly increasing.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jphe.2017.09.02). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Norgard NB, Dinicolantonio JJ. Clopidogrel, Prasugrel, or Ticagrelor? a practical guide to use of antiplatelet agents in patients with acute coronary syndromes. Postgrad Med 2013;125:91-102. [Crossref] [PubMed]
- Hiatt WR, Fowkes FG, Heizer G, et al. Ticagrelor versus Clopidogrel in symptomatic peripheral artery disease. New Engl J Med 2017;376:32-40. [Crossref] [PubMed]
- Shrestha S, Coy S, Bekelis K. Oral antiplatelet and anticoagulant agents in the prevention and management of ischemic stroke. Curr Pharm Des 2017;23:1377-91. [Crossref] [PubMed]
- Linden MD, Tran H, Woods R, et al. High platelet reactivity and antiplatelet therapy resistance. Semin Thromb Hemost 2012;38:200-12. [Crossref] [PubMed]
- Cattaneo M. Diagnosis and management of high platelet reactivity on treatment with Clopidogrel. Semin Thromb Hemost 2012;38:645-51. [Crossref] [PubMed]
- O'Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2013;127:e362-425. [Crossref] [PubMed]
- Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA Guideline Focused Update on Duration of Dual Antiplatelet Therapy in Patients With Coronary Artery Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines: An Update of the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention, 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery, 2012 ACC/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the Diagnosis and Management of Patients With Stable Ischemic Heart Disease, 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction, 2014 AHA/ACC Guideline for the Management of Patients With Non-ST-Elevation Acute Coronary Syndromes, and 2014 ACC/AHA Guideline on Perioperative Cardiovascular Evaluation and Management of Patients Undergoing Noncardiac Surgery. Circulation 2016;134:e123-55. [Crossref] [PubMed]
- Steg PG, James SK, Atar D, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J 2012;33:2569-619. [Crossref] [PubMed]
- Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;130:2354-94. [Crossref] [PubMed]
- Roffi M, Patrono C, Collet JP, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J 2016;37:267-315. [Crossref] [PubMed]
- Capodanno D, Ferreiro JL, Angiolillo DJ. Antiplatelet therapy: new pharmacological agents and changing paradigms. J Thromb Haemost 2013;11:316-29. [Crossref] [PubMed]
- Panak E, Maffrand JP, Picard-Fraire C, et al. Ticlopidine: a promise for the prevention and treatment of thrombosis and its complications. Haemostasis 1983;13:1-54. [PubMed]
- Andrès E, Maloisel F. Idiosyncratic drug-induced agranulocytosis or acute neutropenia. Curr Opin Hematol 2008;15:15-21. [Crossref] [PubMed]
- Savi P, Labouret C, Delesque N, et al. P2Y12, a new platelet ADP receptor, target of Clopidogrel. Biochem Biophys Res Commun 2001;283:379-83. [Crossref] [PubMed]
- Hulot JS, Collet JP, Cayla G, et al. CYP2C19 but not PON1 genetic variants influence Clopidogrel pharmacokinetics, pharmacodynamics, and clinical efficacy in post-myocardial infarction patients. Circ Cardiovasc Interv 2011;4:422-8. [Crossref] [PubMed]
- Tello-Montoliu A, Tomasello SD, Ferreiro JL, et al. Pharmacodynamic effects of Prasugrel dosing regimens in patients on maintenance Prasugrel therapy: results of a prospective randomized study. J Am Coll Cardiol 2012;59:1681-7. [Crossref] [PubMed]
- De Servi S, Goedicke J, Schirmer A, et al. Clinical outcomes for Prasugrel versus Clopidogrel in patients with unstable angina or non-ST-elevation myocardial infarction: an analysis from the TRITON-TIMI 38 trial. Eur Heart J Acute Cardiovasc Care 2014;3:363-72. [Crossref] [PubMed]
- Gurbel PA, Bliden KP, Butler K, et al. Randomized double-blind assessment of the onset and offset of the antiplatelet effects of Ticagrelor versus Clopidogrel in patients with stable coronary artery disease: the Onset/Offset study. Circulation 2009;120:2577-85. [Crossref] [PubMed]
- Nuti SV, Wayda B, Ranasinghe I, et al. The Use of Google Trends in Health Care Research: A Systematic Review. Plos One 2014;9:e109583 [Crossref] [PubMed]
- Crowson MG, Schulz K, Tucci DL. National Utilization and Forecasting of Ototopical Antibiotics: Medicaid Data Versus "Dr. Google". Otol Neurotol 2016;37:1049-54. [Crossref] [PubMed]
- Gahr M, Uzelac Z, Zeiss R, et al. Linking Annual Prescription Volume of Antidepressants to Corresponding Web Search Query Data: A Possible Proxy for Medical Prescription Behavior? J Clin Psychopharmacol 2015;35:681-5. [Crossref] [PubMed]
- Simmering JE, Polgreen LA, Polgreen PM. Web search query volume as a measure of pharmaceutical utilization and changes in prescribing patterns. Res Social Adm Pharm 2014;10:896-903. [Crossref] [PubMed]
- Giorgi MA, Cohen Arazi H, Gonzalez CD, et al. Beyond efficacy: pharmacokinetic differences between Clopidogrel, Prasugrel and Ticagrelor. Expert Opin Pharmacother 2011;12:1285-95. [Crossref] [PubMed]
- Ticlopidine Tablets. Available online: https://www.drugs.com/drug-shortages/Ticlopidine-tablets-661. Last Accessed, June 1, 2017, along with its disappearance from the most recent official guidelines (AHA/ESC).
- Sible AM, Nawarskas JJ. Cangrelor: A New Route for P2Y12 Inhibition. Cardiol Rev 2017;25:133-9. [Crossref] [PubMed]
Cite this article as: Lippi G, Danese E, Bonfanti L, Mattiuzzi C, Cervellin G. Worldwide epidemiology and trends of adenosine diphosphate (ADP) receptor inhibitors usage. J Public Health Emerg 2017;1:76.


