Time to diagnosis, socioeconomic and clinical features of patients with congenital heart diseases in a teaching hospital in Nigeria
Introduction
Congenital heart defects (CHD) are the commonest group of congenital malformation (1). They are the most common cause of infant death occurring from birth defect (2). The incidence of CHDs in developed countries varies from 4 to 50/1,000 live births (3). In Nigerian studies, the incidence of CHDs is 4.6 to 10 per 1,000 live births (4,5).
Studies have shown that there is an increase in the risk of CHDs in lower socioeconomic classes (6,7). Studies with similar findings of higher risk of CHD in low socioeconomic classes have also been reported in Nigeria (4,8).
In studies done in Nigeria 49% to 52.6% of CHD diagnoses were made above 5 years (4,9). These timing of diagnosis is late compare to study by Landis et al. (10) in New York where 68.3% of the babies with CHD had prenatal diagnosis made and 67.2% of babies with CHD had cardiothoracic surgery done before discharge from the neonatal intensive care unit.
A structured and functional referral system is key to effective health care delivery (11). In many developing countries, the tertiary hospitals are usually the first contact of patients to the health care facilities. This results in overburdening of these facilities and high specialist patients load (12).
Sanders et al. (13) in Zimbabwe reported ineffective utilization of the hospital referral system. In the study, only 38% of cases were referred from primary level to the teaching hospital. In Nigeria, there are three levels of health care delivery: the primary, secondary and tertiary health care. Due to poor referral system in Nigeria, a high proportion of patients present to the tertiary health care without referrals is poor. Akande (12) reported as high as 92.9% of cases seen in a tertiary hospital presented without a referral.
Factors such as socioeconomic status and educational achievements are known to affect the health seeking behavior of individuals and their utilization of health care facilities (14,15). However, in a study by Fixler et al. (16) in Texas, no significant relationship was found between the socioeconomic status of caregivers and the timing of diagnosis in children with CHD.
To the best of researchers’ knowledge, no study has been done in Nigeria to ascertain the effect of the socioeconomic status and the referral system on the timing of diagnosis of CHD. Hence, the study aims to describe socioeconomic, clinical features, and time to diagnosis of patients with CHD in a teaching hospital in Nigeria. This will help to educate health policy makers and other stakeholders on the need to increase the awareness of CHD amongst people at risk and also emphasize the need for an effective referral system that will enhance timely diagnosis and specialized care of affected patients.
Methods
This study is a cross-sectional, descriptive study, carried out at the Lagos State University Teaching Hospital (LASUTH), as part of a large study from April 2008 to March 2012. All patients with echocardiography diagnosis of CHD within the study period were included. Patients with prior diagnosis of CHD but that presented at the study period were also included. All patients referred with previous echocardiography of CHD elsewhere were reevaluated in LASUTH by the Paediatric cardiologist.
The subjects were patients with structural heart disease attending the Cardiology clinic of LASUTH. Age at diagnosis was the age at which cardiac evaluation was done and echocardiography diagnosis of CHD was made. Duration of illness was the period from onset of symptoms related to CHD to the time of confirmation of CHD by echocardiography. Duration of illness and age at diagnosis were ages at diagnosis at the referral centres for patients with previous echocardiography diagnosis prior referral (although the diagnosis was confirmed at the current study center before inclusion of such patient in the study). An inclusion criterion was subjects that presented to LASUTH with echocardiography diagnosis of CHD made after evaluation at LASUTH. Subjects with suspected CHD which was ruled out by echocardiography were excluded. All acquired heart diseases were also excluded.
Classification as cyanotic or acyanotic CHD was done following echocardiography findings. Classification as complex heart lesion was done in subjects with more than one heart defect from echocardiography evaluation.
Ethical clearance for this study was obtained from the Research and Ethics Committee of the Lagos State University Teaching Hospital. Informed consent was sought from parents or caregivers of children and also from subjects above eighteen years before enrolment into the study. Assent was also taken from subjects seven years and above.
A structured questionnaire was administered after the aim of the study had been explained to the caregivers/subjects and an informed consent was obtained. A pilot study was carried out with 20 parents to ensure that the questionnaires were easily understood.
The socio-economic stratification was carried out using Oyedeji classification (17). It was determined using maternal education, maternal occupation, paternal education and paternal occupation. The socioeconomic classes were grouped as upper strata for classes I and II, middle stratum for class III and lower strata for classes IV and V. Comparison of the social classes of patients and duration of illnesses were evaluated. All subjects referred and sources of referral were noted in the questionnaire. All self-referred were also noted.
Analysis was done using Microsoft Excel statistical software supplemented by MegaStat statistical package. Patients’ demographics were represented as frequency and percentages. Tables and figures were used to represent those variables as appropriate. Continuous variables were summarized using mean and standard deviation while non-parametric data was summarized using median. Comparison between non parametric data was done using Mann-Whitney’s U test. Kruskal-Wallis test was used to compare the duration of illness before presentation among the studied subjects. Comparison between qualitative data was done using chi square. Probability values less than 0.05 were considered statistically significant.
Results
A total of 300 patients with structural heart disease participated in the study. The age range was 2 days to 35 years with a median age of 13.0 months. Minimum and maximum age at diagnosis of CHD was 2 days and 348 months. Majority (70%) of the subjects were above one year of age. The male:female ratio was 1:1.1. There was a preponderance of Christians among the patients. In the socio-economic distribution of the patients; more than 80% were of middle and lower socioeconomic class.
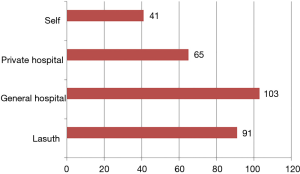
Figure 1 shows the source of referral of the patients, about 15% of the caregivers presented to the tertiary centre on their own without referral.
Fast breathing was the most common presenting complaints (57%) followed by cough (33%) failure to thrive (8.6%) and murmur (7%). Other mode of presentation in these patients included cyanosis (3.7%), presence of other congenital anomalies (3.7%) and easy fatigability (7%).
Table 1 shows the age at presentation of studied subjects. Up to 70% were older than one year at presentation. Over a third (35%) of subjects presented between ages of 60 and 124 months. Up to 21% of subjects had diagnosis of congenital heart disease made after 124 months.
Table 1
| Age groupings (months) | Number of subjects | P value |
|---|---|---|
| 0–12 | 89 | 0.000 |
| 13–59 | 41 | |
| 60–124 | 106 | |
| ˃124 | 64 | |
| Total | 300 |
There was no statistically significance difference in the various social groups in the duration of illness before presentation. 45% of the subjects had been admitted at least once.
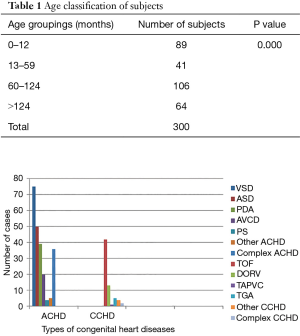
Figure 2 shows the echocardiography categories of acyanotic and cyanotic congenital heart diseases that was seen in subjects. Cyanotic congenital heart disease was seen in seventy-one subjects (23.7%) while 76.3% had echocardiography diagnosis of acyanotic heart lesion. The three commonest acyanotic congenital heart diseases are ventricular septal defect (32.7%), atrial septal defect (21.8%) and patent ductus arteriosus (17%). The commonest cyanotic CHD were tetralogy of Fallot (63.4%) and double outlet right ventricle (18.3%).
Five subjects classified as other acyanotic heart disease were three cases of aortic stenosis, a case of dextrocardia and an infant with hypertrophy cardiomyopathy. Classification of other cyanotic heart disease included five cases of truncus arteriosus, two cases of tricuspid atresia and a case of hypoplastic left heart syndrome.
Subjects classified as complex heart lesion were those with two or more echocardiography of heart diseases. Complex acyanotic congenital heart disease was seen in 36 (15.7%) of subjects with acyanotic heart lesion. Out of subjects with complex acyanotic heart lesion, there were seven cases of ventricular septal defect and patent ductus arteriosus. Four subjects had atrial septal defect and ventricular septal defect. Other complex lesion seen were atrial septal defect with patent ductus arteriosus, atrioventricular canal defect with patent ductus arteriosus and three or more cardiac anomalies. Two cases of complex cyanotic heart diseases were combination of Tetralogy of Fallot and atrial septal defect and a case of truncus arteriosus and ventricular septal defect.
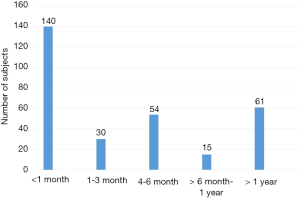
Figure 3 shows the duration of illness before presentation. Less than half of the subjects presented within 1 month after birth (46.6%). Up to 20% presented more than 1 year after the onset of illness.
Table 2 shows the reclassification of subjects with acyanotic congenital heart disease according to age group. About one-third (33.3%) cases of ventricular septal defect were diagnosed in infancy. In all except pulmonary stenosis, more than half of the subjects had diagnosis of congenital heart disease after infancy. A high proportion of subjects (10–26%) except in cases with pulmonary stenosis had echocardiography diagnosis of acyanotic heart lesion after age of 124 months.
Table 2
| Cardiac lesions | 0–12 months (%) | 13–59 months (%) | 60–124 months (%) | >124 months (%) | Total (100%) | Statistics |
|---|---|---|---|---|---|---|
| VSD | 25 (33.3) | 10 (13.3) | 22 (29.3) | 18 (24) | 75 | ᵡ2=28.55; P value =0.054 |
| ASD | 19 (38) | 7 (14) | 11 (22) | 13 (26) | 50 | |
| PDA | 5 (12.8) | 6 (16.7) | 20 (51.3) | 8 (20.5) | 39 | |
| PS | 3 (75) | 1 (25) | 0 (0) | 0 (0%) | 4 | |
| AVCD | 4 (20) | 7 (35) | 7 (35) | 2 (10) | 20 | |
| Other ACHD | 1 (20) | 0 (0) | 3 (60) | 1 (20) | 5 | |
| Complex ACHD | 15 (41.6) | 6 (16.6) | 10 (28.8) | 5 (13.9) | 36 |
VSD, ventricular septal defect; ASD, atrial septal defect; PDA, patent ductus arteriosus; PS, pulmonary stenosis; AVCD, atrioventricular canal defect; ACHD, acyanotic congenital heart disease.
Table 3 shows the reclassification of cyanotic congenital heart diseases according to age groupings. Most cases had echocardiography diagnosis made between 60 and 124 months. However, 60% of transposition of great arteries was diagnosed in infancy while complex heart lesions were seen in an infant and a 26-month old toddler.
Table 3
| Cardiac lesions | 0–12 months (%) | 13–59 months (%) | 60–124 months (%) | >124 months (%) | Total (100%) | Statistics |
|---|---|---|---|---|---|---|
| TOF | 6 (14.3) | 2 (4.8) | 23 (54.7) | 11 (26.2) | 42 | ᵡ2=18.68; P value =0.229 |
| DORV | 3 [23] | 1 (7.7) | 7 (53.8) | 2 (15.4) | 13 | |
| TAPVC | 0 (0) | 0 (0) | 1 (100) | 0 (0) | 1 | |
| TGA | 3 (60) | 1 (20) | 1 (20) | 1 (20) | 5 | |
| Other CCHD | 4 (50) | 0 (0) | 0 (0) | 4 (50) | 8 | |
| Complex CCHD | 1 (50) | 1 (50) | 0 (0) | 0 (0) | 2 |
TOF, Tetralogy of Fallot; DORV, double outlet right ventricle; TAPVC, total anomalous pulmonary venous return; TGA, transposition of great arteries; CCHD, cyanotic congenital heart disease.
Discussion
The mean age ± standard deviation of 32.50±48.06 months diagnosis of CHD of patients in this study is high compared with the western world and even some developing countries like India where diagnosis is made in utero (18). It is also higher than that reported from Turkey (19), Kenya (20) and an earlier report from Nigeria by Ibadin (4), however it is comparable to the mean age at diagnosis reported from Yemen (21) and an earlier report by in the same region with the current study (5). A higher mean age may translate to a significant number of patient not having optimal surgical intervention (20).
Although the median age of the patients at diagnosis in this report is about 13 months, only 43% had diagnosis before 5 years. This is worrisome as these are defects which has been present before birth and which mostly manifests with symptoms at the neonatal period and infancy and is sometimes severe enough to affect feeding and hence growth of the infant and sometimes is responsible for infant death and the need for early presentation and diagnosis is important (4,18).
No significant gender differences among the patients in this report with male to female ratio of 1:1.1. The finding in the present study is not different from earlier reports (4,19,21).
Although there were more Christians among the parents and adult subject, the immediate reason for this finding is not clear as the study region has a mixture of population from various part of the country. The authors are not aware of any previous report which has documented effect of religion on presentation to the hospital hence may conclude that this was an incidental finding. Up to 15% of the respondents presented to the study centre on their own as a first point of call without referral from either primary or secondary health centres, even though the study centre is a tertiary centre. This is far from ideal as practiced in the Western world but may be a reflection of the practices in the tertiary health centres in the region. Why will parent prefer to come to the tertiary centre as a first point of call? Could it be that the primary and secondary centres are not well developed in terms of facility and manpower? Could it also be lack of awareness of the ideal referral chain by the parent? It would have been expected that parent will present at the primary health centre first who is expected to be closer to their reach, where cases that can’t be handled there will then be referred to the secondary centres by the specialist, from where more difficult cases can then be referred to tertiary centres for detailed investigation and management. The trend here may tend to weary the tertiary centre who then may not be able to give appropriate attention to the difficult cases meant for her by the time they present.
Fast breathing, cough, failure to thrive and murmur were the presenting complaints in order of decreasing frequency as in a previous Nigerian report (4). Fast breathing in congenital heart disease can be as a result of increased blood flow to the lungs causing engorgement of the pulmonary vascular beds resulting in interstitial edema. The excess fluid in the lung tissues will therefore act as a barrier for proper gaseous exchange, rendering the process less effective. To compensate the respiratory rate and effort increases manifesting as respiratory distress (22).
Failure to thrive is because patients with respiratory distress and poor cardiac output due to heart disease cannot feed well as it requires considerable effort to suckle resulting in easy fatigability and failure to thrive. It is also due to increase basic metabolic rate associated and decrease intake, hence the consumption of calories outweighs the caloric intake (23).
Murmur is due to turbulence of blood flow as a result of Pressure difference between two structures during systole and diastole. Cough may be due to pulmonary congestion which predisposes them to recurrent respiratory tract infection (22).
In the current study up to half of the patient presented within three months of the onset of illness but it is still high and quite disturbing that about 20% actually presented after one year of the onset of illness. In comparison with a study by Keuffer et al. (24) in Switzerland where late diagnosis was mostly at age range of 4 months to 6 months, there is need for institution of measures required for early identification of cases of congenital heart diseases in Nigeria. The reason for this may be explained by the fact that most of the respondents belong to the middle and lower socioeconomic class, maternal education has been found to have prominent effect of the prognosis of illness in a patient (25). It is expected that an educated mother is likely to note on time about a child’s illness and seek help in the right place; unfortunately, in the current report socioeconomic class did not have any significant effect on duration of illness before presentation. The reason for this is not immediately clear but could be due to the fact that many of the parents in the higher socioeconomic classes are also busy with career and work hence may not find enough time to present to the hospital early, or is it that education has not translated to information especially on health.
In conclusion this study showed that patient with structural heart disease in this region often present late regardless of their socioeconomic classes leading to delayed diagnosis. The proportion who had self-referral was high. Fast breathing, cough, failure to thrive and murmur were the presenting complaints in order of decreasing frequency. There is a need to develop an educational program to increase awareness on the symptoms suggestive of congenital heart disease and importance of early presentation. There is also a need to develop a referral chain among health system in the region.
Acknowledgments
We gratefully acknowledge the subjects who participated in this study, their parents and caregivers including other staff who were involved in their care.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jphe.2018.04.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Lagos State University Teaching Hospital (LREC.06/10/823). Informed consent was taken from all subjects.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Tennant PW, Pearce MS, Bythell M, et al. 20-year survival of children born with congenital anomalies: a population-based study. Lancet 2010;375:649-56. [Crossref] [PubMed]
- Yang Q, Chen H, Correa A, et al. Racial differences in infant mortality attributable to birth defects in the United States, 1989-2002. Birth Defects Res A Clin Mol Teratol 2006;76:706-13. [Crossref] [PubMed]
- Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol 2002;39:1890-900. [Crossref] [PubMed]
- Ibadin MO, Sadoh WE, Osarogiagbon W. Cogenital heart diseases at the University of Benin Teaching Hospital. Niger J Paediatr 2005;32:29-32.
- Okoromah CA, Ekure EN, Ojo OO, et al. Structural heart disease in children in Lagos: profile, problems and prospects. Niger Postgrad Med J 2008;15:82-8. [PubMed]
- Mughal AR, Sadiq M, Hyder SN, et al. Socioeconomic status and impact of treatment on families of children with congenital heart disease. J Coll Physicians Surg Pak 2011;21:398-402. [PubMed]
- Yu D, Feng Y, Yang L, et al. Maternal socioeconomic status and the risk of congenital heart defects in offspring: a meta-analysis of 33 studies. PLoS One 2014;9:e111056 [Crossref] [PubMed]
- Animasahun A, Kehinde O, Falase O, et al. Caregivers of children with congenital heart disease: Does socioeconomic class have any effect on their perceptions? Congenit Heart Dis 2015;10:248-53. [Crossref] [PubMed]
- Kolo PM, Adeoye PO, Omotosho AB, et al. Pattern of congenital heart disease in Ilorin, Nigeria. Niger Postgrad Med J 2012;19:230-4. [PubMed]
- Landis BJ, Levey A, Levasseur SM, et al. Prenatal diagnosis of congenital heart disease and birth outcomes. Pediatr Cardiol 2013;34:597-605. [Crossref] [PubMed]
- World Health Organization/UNICEF: Primary Health Care.’' Health for all'' Geneva, World Health Organization, 1978;1:64.
- Akande TM. Referral system in Nigeria: Study of a tertiary health facility. Ann Afr Med 2004;13:130-13.
- Sanders D, Kravitz J, Lewin S, et al. Zimbabwe’s hospital referral system: does it work? Health policy and planning. Health Policy Plan 1998;13:359-70. [Crossref] [PubMed]
- Daly MC, Duncan GJ, McDonough P, et al. Optimal indicators of socioeconomic status for health research. Am J Public Health 2002;92:1151-7. [Crossref] [PubMed]
- Owoseni JS, Jegede LI, Ibikunle AM. Socio-economic status and utilization of healthcare facilities in rural Ekiti, Nigeria. Stand Res J Med Sci 2014;2:001-43.
- Fixler DE, Pastor P, Sigman E, et al. Ethnicity and socioeconomic status: impact on the diagnosis of congenital heart disease. J Am Coll Cardiol 1993;21:1722-6. [Crossref] [PubMed]
- Oyedeji GA. Socio-economic and cultural background of hospitalized children in Ilesha. Niger J Paed 1985;12:111-7.
- Mocumbi AO, Lameira E, Yakish A, et al. Challenges on the management of congenital heart disease in developing countries. Int J Cardiol 2011;148:285-8. [Crossref] [PubMed]
- Başpinar O, Karaaslan S, Oran B, et al. Prevalence and distribution of children with congenital heart diseases in the central Anantolian region, Turkey. Turk J Pediatr 2006;48:237-43. [PubMed]
- Awori MN, Ogendo SW, Gitome SW, et al. Management pathway for congenital heart disease at Kenyata National Hospital, Nairobi. East Afr Med J 2007;84:312-7. [PubMed]
- Saleh HK. Pattern of congenital heart disease in Southern Yemeni children referred for echocardiography. Saudi Med J 2009;30:824-8. [PubMed]
- World Health Organization. Pocket Book of Hospital Care for Children: Guidelines for the Management of Common Childhood Illnesses. 2nd edition. Geneva USA, 2013.
- Block RW, Krebs NT. Failure to thrive, development, child neglect, abuse, nutrition. Paediatrics 2005;116:1234-7. [Crossref]
- Keuffer A, Pfammatter J. Timely diagnosis of congenital heart disease - did we improve? Cardiovascular Medicine 2015;18:282-4. [Crossref]
- Desai S, Alva S. Maternal education and child health: is there a strong causal relationship? Demography 1998;35:71-81. [Crossref] [PubMed]
Cite this article as: Animasahun BA, Adekunle MO, Kusimo OY. Time to diagnosis, socioeconomic and clinical features of patients with congenital heart diseases in a teaching hospital in Nigeria. J Public Health Emerg 2018;2:15.