COVID-19 spread, wildlife protection and the response capacity on public health crisis: empirical research of 31 provinces and cities in China
Introduction
In December 2019, a number of cases of unexplained pneumonia were found in the Huanan seafood market located in Wuhan, Hubei Province, China, who showed symptoms such as persistent fever, cough, shortness of breath, chest radiographs showing invasive lesions of both lungs, and were positive for nucleic acid testing (1). After monitoring by Chinese health authorities, it was found that the unexplained pneumonia was an infectious disease caused by a novel coronavirus, with an incubation period of 2 to 14 days (2,3). Coronavirus disease 2019 (COVID-19) is an acute respiratory infectious disease caused by respiratory tract and contact infection, with short transmission time, strong transmissibility, and characteristics of human-to-human transmission (4). Previous studies have shown that new infectious diseases such as bird flu, Ebola, and Middle East respiratory syndrome, which have appeared in recent years around the world were related to animals, and COVID-19 is no exception.
In January 2020, a large number of patients sought medical treatment in Wuhan, and death cases occurred. Wuhan imported cases were successively found in 18 countries such as Thailand. The epidemic spread rapidly. In view of this, the Chinese government launched an emergency plan, in order to prevent a large number of population movements during the Lunar New Year holiday season and effectively control the infectious epidemic, it was decided to close Wuhan on January 23, comprehensively investigate the sick population, and provide admission and assistance. On the morning of January 31, Beijing time, the World Health Organization (WHO) also voiced that the novel coronavirus was classified as a public health emergency of international concern (PHEIC) (5). The Chinese government is beginning to realize the importance of strengthening wildlife protection and public health emergency management.
With the rapid development of the epidemic, 31 provinces, cities and autonomous regions in China have successively experienced confirmed and suspected cases, and experts from the High-Level Expert Group of the National Health Commission called on the people not to flow during the holiday season and consciously isolate them at home for 7–14 days. In this paper, we will systematically analyze and sort out the epidemic development in the next 14 days and the intervention measures taken by China to deal with the public health crisis. January 24, the first day of the Lunar New Year holiday, also the first day of the initiation of emergency measures in China is the starting point for discussion.
Methods
As of February 15, 2020, there are over 60,000 confirmed cases and 1,000 plus deaths. Since the first provinces to initiate the level I response started on January 23, 2020, the incubation period of the virus is 14 days. Therefore, this article has counted the changes of the virus infected people from January 24th to February 7th, as well as the newly diagnosed, cumulatively diagnosed, dead and cured cases in the whole country and 31provinces. Data and sources are form the official website of provincial health committees and the National Health Commission of China. We use SPSS software for descriptive statistical analysis use GeoDa software draw Epidemic map of provinces in China.
In order to explore the emergency response measures issued by the provinces and departments, this study also analyzes the policy texts and lists them based on the relevant information from the government websites of each department and province.
Results
Overall epidemic status and spread trend
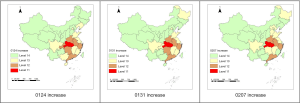
As shown in Figure 1, the first day was January 24 and the 15th day was February 7. The data on the main coordinates show an increase in the daily number of confirmed cases (increase), a cumulative total of confirmed cases (total), and a cumulative number of suspected infections (suspect). The data on the secondary axis shows the cumulative death toll (death) and the cumulative cured cases (cured). Overall, the cumulative number of confirmed cases, the cumulative number of deaths and the cumulative number of cured are rising. The cumulative confirmed cases (red line) and cumulative death cases (yellow line) both showed an approximately linear growth pattern. At the same time, the growth rate of cumulative confirmed cases was greater than that of cumulative death cases. The cumulative cured cases (green line) showed an approximately exponential growth pattern. With the development of government emergency measures and the progress of medical technology, people have a deeper understanding of diseases, and various medical measures are more appropriate and effective, and the mortality rate is decreasing.
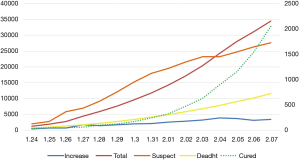
On the 9th day (January 31), there was a crossover between the number of people discharged and the number of deaths, the first time the number of people discharged was greater than the number of deaths. Since that day, the slope has been climbing, which means that the rate of growth has been rising. The cumulative number of confirmed cases and the cumulative number of suspected cases crossed on the 12th day, and the slope of confirmed cases became larger and the slope of suspected cases became smaller. This suggests that the status of many suspected patients has finally been confirmed due to the deepening understanding of the virus among medical staff. On the other hand, it also shows that the growth rate of suspected infected people is decreasing with the emergency policy of the government. The decrease in the number of new diagnoses on the 13th day (February 5), suggests that there is no immediate effect after the start of the emergency response, but rather a period of response. The occurrence of these intersections points indicates that infection has been effectively controlled to a certain extent, and although the absolute number of suspected infections and deaths is still increasing, there is a tendency for the growth rate to decrease.
Epidemic situation in each Province
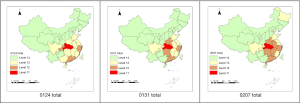
By consulting the provincial health committees and the official website of National Health Commission of China, this thesis counts the newly confirmed and cumulative confirmed cases in each province from 00:00 on January 24 to 24:00 on February 7. Because the data are updated every day and the time interval is relatively long, this paper chooses three-time nodes to draw the growth map and the total map respectively. The three time points are January 24, January 31 and February 7 respectively. The reason why this article chose these three-time nodes is that from the afternoon of January 23, each province announced that it would start the level I response from 00:00 on January 24. Moreover, on the evening of January 30, the World Health Organization announced that the outbreak of Novel coronavirus pneumonia was listed as a PHEIC. January 31 is exactly one week away from it, and the total number of confirmed cases at this time point exceeded 10,000 for the first time. On February 7, the interval was another week, at which point a complete observation of the latent period (14 days) was completed.
In this paper, we use ArcGIS software to draw spatial distribution maps. This software can automatically identify the peak and valley areas of the value, which is more suitable for a comprehensive analysis of 31 provinces. As the Chinese government generally divides 31 provinces into four levels in the process of crisis management and risk management, this article draws a quartile map. Figure 2 shows the number of new diagnoses and the quartile map at the three time points (compared to the previous day). In the process of data processing, There are four grades according to the size of the new number in 31 provinces and cities and Hong Kong, Macao and Taiwan regions: the first grade represents a very large number of increase, which needs to be kept under control; the fourth grade represents a relatively small amount of increase, we’ve almost got the infection under control. Red, orange, yellow and green represent the first, second, third and fourth grades respectively. At the three time points, the red areas are all Hubei Province, which shows the most obvious trend of increase in the number of infected people, which will be specifically analyzed below. On January 24, the orange areas were Henan, Anhui, Zhejiang, Chongqing, Hunan, Guangdong and six other provinces. On January 31, the orange areas were Henan, Anhui, Zhejiang, Hunan and Guangdong provinces. Chongqing turned yellow. On February 7, the orange areas were Henan, Anhui, Zhejiang and Guangdong provinces, Chongqing became green, and Hunan became yellow. This shows that Hubei is the core area of the epidemic, the surrounding provinces infection rates are relatively high. From January 24 to February 7, the increase in the number of infected people from the previous day has been brought under control, and the orange areas have begun to decrease, and the yellow and green areas have begun to increase.
Figure 3 shows the total number of confirmed cases at the three time points. According to the number of confirmed cases in each province and region, we divided them into 4 grades: the first grade indicates that the cumulative number of confirmed cases is very large, and the epidemic situation is very serious. By analogy, level 4 indicates a cumulative number of confirmed fewer people, the total number of infections is not much. Red, orange, yellow and green represent grades one, two, three and four respectively. Of the three time points, the red areas are all Hubei Province, which indicates that Hubei Province is the worst affected area with the largest number of confirmed cases. On January 24, the orange areas were Chongqing, Zhejiang and Guangdong. On January 31, the orange areas were Henan, Hunan, Guangdong and Zhejiang provinces. On February 7, the orange areas were Henan, Anhui, Zhejiang, Hunan, Jiangxi, and Guangdong provinces. In the process, Chongqing went from orange to yellow. And Henan, Anhui, Hunan and Jiangxi went from yellow to orange. The provinces with the highest number of confirmed cases are all neighboring provinces of Hubei except Guangdong. Chongqing’s overall population is growing at a relatively slower rate than that of other provinces bordering Hubei. This shows that the spread of the epidemic has a certain “geographical”. Although Guangdong is not adjacent to Hubei Province, it is the main place of outflow and import of Hubei population, so its epidemic situation is also more serious. This shows that the spread of the epidemic affected by economic factors, social factors, and the combined impact of population movements.
The situation of Hubei Province and the measures taken
The origin of this epidemic is from Wuhan, the capital city of Hubei province. Therefore, the growth rate and the accumulative total number of confirmed cases of Hubei all rank on the top in China. Therefore this article needs to carry on the separate review and the special research to Hubei Province. The first confirmed case officially recorded in Hubei Province occurred in December 2019. On January 1, 2020, the Hubei Provincial Government shut down Huanan seafood market. On January 9, the first death case occurred in Hubei Province. At 24:00 on January 10, Hubei Province reported to the National Health Commission of China, which completed the detection of pathogenic nucleic acids. On January 22, the Hubei provincial government held the first press conference on the epidemic prevention and control work of Novel coronavirus pneumonia. On January 23, National Health Commission of the People’s Republic of China organized the formulation of Technical Guidelines for Prevention and Control of Infection of Novel coronavirus pneumonia in Medical Institutions (First Edition), requesting local health administrative departments at all levels to designate special personnel to be responsible for the prevention and control of infections in medical institutions within their jurisdiction, so as to minimize the risk of transmission of Novel coronavirus pneumonia in medical institutions. As of 00:00 on January 23, 17 death cases in China all came from Hubei. These deaths were all middle-aged patients over 45 years old, aged 48–89 years old, and most of them had previous medical history, such as hypertension, diabetes and other chronic diseases. On January 24, the Hubei government launched a level I emergency response and issued a public notice calling on the elderly and people with chronic diseases and other immunocompromised people to live at home and not to enter or leave public places. After the emergency response was initiated, the cumulative number of confirmed cases in Hubei province was 729 at 24:00 on January 24, with 39 deaths, 32 discharges, 5.35% mortality and 4.39% cure rate. At 24:00 on January 31, the cumulative number of confirmed cases in Hubei Province was 7,153, the death toll was 249, the number of discharged patients was 166, the mortality rate was 3.48%, and the cure rate was 2.32%. The main reason for the decrease in mortality rate and cure rate was that the society had effectively avoided the aggravation of the patient's illness at this time as all sectors of society had deepened their understanding of the epidemic disease. However, as the number of confirmed and suspected cross-infection patients has increased, the absolute number has increased again and the cure rate has also decreased.
China’s health authorities and the Hubei provincial government are beginning to realize that COVID-19 has a lower mortality rate than SARS, but that its infection rate is very high and its concealment is very strong. Therefore, the diagnosis and treatment are based on the characteristics of the disease to improve. Therefore, the way of diagnosis was changed from simple nucleic acid detection to combine CT and nucleic acid detection, in order to improve the timeliness and accuracy of detection. In addition, the government has made the control and reduction of the infection rate the top priority of the epidemic prevention and control work. At the same time, the Wuhan government began to copy the SARS-era “Xiaotangshan Hospital” to build a special hospital to deal with infectious diseases. On February 2, The Fire God Mountain Hospital was built and quickly put into use, a step that has greatly reduced the rate of disease transmission and increased the rate of cure. On February 6, the Thunder God Mountain Hospital passed the acceptance and gradual transfer to use. On February 7, 24,953 people were diagnosed, 699 died, 1,115 were discharged, the mortality rate was 2.80%, the cure rate was 4.47%. Compared with January, the mortality rate in Hubei Province has decreased significantly, and the cure rate has increased significantly in February. As of February 7, the Hubei provincial government held a total of 17 press conferences, during which administrators and professionals from government departments and medical institutes were invited to report on the prevention and control of the epidemic, and the public’s right to know and to supervise is guaranteed.
The relationship between COVID-19 and wildlife protection
Scientific research shows that new infectious diseases such as bird flu, Ebola, and Middle East respiratory syndrome, which have appeared in recent years around the world, are related to animals. These viruses originally exist in nature, wildlife hosts do not necessarily cause disease and death. However, when humans eat wild animals or erode wildlife habitats, the contact between these viruses and humans has increased significantly, causing the virus to spread from wildlife to humans. Endangering public health and safety. Previous studies have shown that the host of COVID-19 pneumonia is likely to be various wild animals, including pangolins, bats, snakes, and so on (6-9).
Containing biodiversity loss and promoting environmental sustainable development, and ensuring healthy lifestyles and promoting well-being for people at all ages are the two key goals of the UN’s 2030 agenda for sustainable development. In January 2019, in the face of increasing risks of high-consequence and globally catastrophic biological events, The Global Health Security (GHS) Index is the first comprehensive assessment and benchmarking of health security and related capabilities across the 195 countries that make up the States Parties to the International Health Regulations [IHR (2005)]. This index will spur measurable changes in national health security and improve international capability to address one of the world’s most omnipresent risks: infectious disease outbreaks that can lead to international epidemics and pandemics (10). Biological threats in any country can pose risks to global health, international security, and the worldwide economy. Infectious diseases caused by it know no borders, all countries must prioritize and exercise the capabilities required to prevent, detect, and rapidly respond to public health emergencies. Every country also must be transparent about its capabilities to assure neighbors it can stop an outbreak from becoming an international catastrophe. The specific contents of the GHS index and its global mean are shown in Table 1. The final result of GHS index shows that the overall mean of 195 countries is only 40.2 out of 100. China’s overall score on the six indicators was 48.2, slightly above the global average and 51st out of 195 countries. Of the six categories, China scored the highest, at 64.4, for the country’s overall risk and vulnerability to biological threats.
Table 1
| No. | Indicator | Weight | Mean | China | Rank |
|---|---|---|---|---|---|
| 1 | Prevention of the emergence or release of pathogens (prevention) | 16.30% | 34.8 | 45.0 | 50 |
| 2 | Early detection and reporting for epidemics of potential international concern (detection and reporting) | 19.20% | 41.9 | 48.5 | 64 |
| 3 | Rapid response to and mitigation of the spread of an epidemic (rapid response) | 19.20% | 38.4 | 48.6 | 47 |
| 4 | Sufficient and robust health system to treat the sick and protect health workers (health system) | 16.70% | 26.4 | 45.7 | 30 |
| 5 | Commitments to improving national capacity, financing plans to address gaps, and adhering to global norms (norms) | 15.80% | 48.5 | 40.3 | 141 |
| 6 | Overall risk environment and country vulnerability to biological threats (risk environment) | 12.80% | 55.0 | 64.4 | 58 |
Resource from 2019 Global Health Security Indicators. GHS, Global Health Security.
The core finding of the report is that no country in the world is fully prepared for pandemics and severe outbreaks, and every country has weaknesses that need to be addressed. The report argues that there is little evidence that most countries have proven important health security capabilities or that they can play a role in a crisis. Only 11 per cent of countries have a medical response to deal with the health emergency event and the majority countries lack the capacity to respond to a pandemic. Thirty-one percent of countries do not have cross-border agreements for public health emergency responses, so as promoting compliance with international health and security norms is become critical. The report also showed that more than two-thirds of the viruses were transmitted from animals to people at first and became human-to-human transmission. However, the health management systems for people, animals and the environment are fragmented across different sectors. Currently, there is a lack of coordinated communication and professional training among public health professionals, wildlife experts, veterinarians, and management decision makers, and only 30 percent of countries have established data-sharing mechanisms between human, animal, and wildlife monitoring authorities. Then we analyze China’s efforts and existing problems in wildlife protection and emergency management in the next part.
Wildlife protection and emergency responses in 31 provinces
In terms of China’s emergency management system, China’s emergency control is mainly replying on state-led management, in other words, the emergency response system is made up from “state-province-city-county” four-level organizational sections (11). This article will focus on introducing and analyzing wildlife protection system built and the necessary emergency measures taken by provincial and government departments for outbreak control.
In the current legal system, China’s laws directly related to wildlife including Wildlife Protection Law, Animal Disease Prevention law, the law about quarantine of animals and plants, and so on. The most important of these is the wildlife protection law. Although the Wildlife Protection Law has related prohibitions on the consumption and trading of wild animals, it clearly stipulates that the purchase or trading of precious and endangered wild animals constitutes a crime, but the scope of the prohibition is relatively small, and there are still blind spots in the relevant regulations, making it difficult to control public health risks. Because the objects protected by the Wildlife Protection Law are mainly precious and endangered species, not all wildlife are included in the scope of protection. A large number of high-risk animals carrying the virus are not under management and protection, including bats, rodents and other high-risk species that spread the disease. There is no legal regulation on the behavior of simply eating these animals, and people are only prohibited from eating wild animals on a moral level. The effect is very limited. On February 3, 10 ministries (bureaus) including The State Administration for Market Regulation, The Ministry of Ecology and Environment of P.R.C jointly deployed special enforcement actions to combat wildlife illegal transactions, implemented the most stringent control measures and prohibiting all forms of wildlife trade. Some provinces and cities have begun to promote local legislation after the outbreak. For example, Hunan Province upgraded its wildlife control measures and issued an official document on February 10, it is forbidden to eat wild animals across the province, prevent wild animals from flowing to the table from the source, and prevent cross-infection transmission of disease. Tianjin also introduces policy bans eating and trading wild animals on February 14, 2020. Many places have stated in official documents that it is forbidden to eat and trade wild animals.
COVID-19 pneumonia epidemic highlights the importance and urgency of wildlife protection. As a non-traditional security factor, the impact of biosecurity on human security and national security has been increasing in recent years. For example, SARS, Ebola, African swine fever and other infectious disease outbreaks caused by natural hosts, foodborne diseases and animal diseases pose serious threats to human health. The invasion of alien species has disrupted biodiversity and left the ecosystems on which humans depend to face many challenges. While the rapid development of biotechnology has brought benefits to human beings, it has also brought unprecedented scientific and technological ethical dilemmas and security risks. From an international perspective, China has proactively assumed international responsibility for safeguarding biosafety, signed the Convention on Biological Diversity, and ratified the Cartagena Protocol on Biosafety to the Convention on Biological Diversity. From a domestic perspective, China has successively formulated a series of laws and policies related to wildlife protection, including the Wildlife Protection Law and the Communicable Disease Control Law. In October 2019, China’s draft biosafety law was also submitted for review for the first time. In the future, it is necessary to introduce special laws related to biosafety and wildlife protection, combining wildlife protection with public health and the construction of national security system.
The Chinese Lunar New Year is the largest annual mass travel event worldwide, risking amplification of the spread of COVID-19. In response, the provinces of mainland China has been to initiate the level I response to major public health emergency. General Emergency Plan for National Public Emergencies of China and Contingency Plan for National Work Safety Accidents and Disasters of China classify accident response into four levels, namely, Grade I accident (level I response), Grade II accident (level II response), Grade III accident (level III response) and Grade IV accident (level IV response). The grade I accident indicates that the cumulative number of confirmed cases is very large, and the epidemic situation is very serious. By analogy, level 4 indicates a cumulative number of confirmed fewer people. In addition, all levels of the government, health administrations, medical institutions, disease prevention and control institutions, health supervision institutions, entry-exit inspection and quarantine institutions and non-incident areas must take measures to response the accident. The “level I response” is the highest level. In the event of a major public health emergency, the provincial headquarters shall organize and coordinate the emergency handling work within its administrative area in accordance with the decision-making arrangement and unified command of the State Council. In the emergency response state, authorities have closed public transit and cancelled outbound transportation (air, train, and long-haul buses). Vehicular traffic in Wuhan was banned. China also imposed a ban on overseas travel with tour groups and suspended sale of flight and hotel packages. Authorities cancelled Lunar New Year gatherings as well as intraprovince bus service in some provinces (12).
The time nodes for initiating the level I response in 31 provinces of the mainland China are shown in Table 2. Zhejiang, Guangdong and Hunan were among the first three provinces to initiate a level I response, mainly because the confirmed cases were detected earlier in all three provinces, and all of these cases were imported cases from Hubei Province (imported cases refer to travel from Hubei Province to the region, where they were diagnosed, treated or infected). The Spring Festival travel season in China kicked off on January 10. While Hunan was the province adjacent to Hubei, Zhejiang and Guangdong are economically developed provinces with very large net population inflow and population flow. In the Spring Festival travel season, these three provinces would inevitably flow into a large number of Wuhan permanent residents. As a result, the three provinces were the first to enter a level I response state. The city of Wuhan was closed on January 23, but before the closure there was a massive influx of people into other provinces, and the spread of imported cases has led other provinces to initiate a level I response. On January 24, a further 14 provinces launched a level I response, including Hubei Province and its neighboring provinces and cities such as Anhui and the four municipalities. On January 25, 13 provinces were added. Emergency measures have not been activated in Tibet since no confirmed cases have been detected during this period. The first case was confirmed in Tibet on January 29, and a level I response was announced. At this point, all 31 provinces in mainland China have entered a state of level I response.
Table 2
| Date | Provinces announced level I emergency response | Grand total |
|---|---|---|
| Jan 23 | Zhejiang, Guangdong, Hunan | 3 |
| Jan 24 | Hubei, Anhui, Tianjin, Beijing, Shanghai, Chongqing, Sichuan, Jiangxi, Yunnan, Guizhou, Shandong, Fujian, Guangxi, Hebei | 17 |
| Jan 25 | Jiangsu, Hainan, Xinjiang, Henan, Heilongjiang, Gansu, Jilin, Liaoning, Shanxi, Shaanxi, Qinghai, Ningxia, Inner Mongolia | 30 |
| Jan 29 | Tibet | 31 |
The emergency response measures taken by national departments
The response to the epidemic situation involves the cooperation of health administrative authorities, transportation authorities, financial authorities and other parties. National government departments have successively taken necessary countermeasures to maximize the supply of materials and reduce patient pressure and large-scale population movement (See Table 3).
Table 3
| Time | Department | Measures |
|---|---|---|
| Jan 11–Feb 6 | National Health Commission of China | Monitoring and releasing the epidemic situation to the nation |
| Listing COVID-19 as class B infectious disease and taking class A infectious disease prevention and control measures | ||
| Managing and controlling COVID-19 accordance to the Frontier health and Quarantine Law of the people’s Republic of China | ||
| Issued the second to fourth edition of the Plan for Prevention and Control of COVID-19 Pneumonia | ||
| Jan 22 | National Healthcare Security Administration | Adopting the special reimbursement policy to confirmed COVID-19 patients |
| Jan 23 | Ministry of Transport of P.R.C, China Railway, Civil Aviation Administration of China | From the midnight on January 24, 2020, passengers who have purchased train tickets, bus tickets, ship tickets and air tickets before this date will be waived refund fees if they voluntarily change their itinerary and need to refund |
| Jan 27 | Ministry of Finance of P.R.C, National Health Commission of P.R.C | In 2020, the central government of China allocated 60.33 billion Yuan of subsidies for essential public health services and epidemic prevention and control at the grassroots level in total |
| Ministry of Education of P.R.C | Issued and released the notice on the extension of the spring semester in 2020 to Universities, Colleges, Primary and Secondary Schools, and Kindergartens, and training schools |
COVID-19, coronavirus disease 2019.
Since the issuance of the second edition to fourth edition of the Pneumonia Prevention and Control Plan for New Coronavirus Infection by the CDC of the National Health Commission from January 22 to February 6, it is clearly specified that the working principles of “prevention first, prevention and control combined, scientific guidance, and timely treatment” should be adopted. And it is required that governments at all levels and health administrative authorities at all levels should strengthen the guidance for the prevention and control of local epidemic situations, establish a technical expert group for prevention and control, formulate and improve the relevant work and technical plans, and further standardize the pneumonia prevention and control for new coronavirus infection. The health and health administrative authorities at all levels shall be responsible for the overall guidance for epidemic control and implement the prevention and control funds and materials. The rapid control institutions at all levels shall be responsible for organizing, coordinating, supervising and evaluating the monitoring work, collecting, analyzing, reporting and feeding back the monitoring data; carrying out on-site investigation, laboratory testing and professional technical training; and carrying out health education and risk communication for the public. Medical institutions at all levels and at all levels shall be responsible for case detection and reporting, isolation, diagnosis, treatment and clinical management, carry out specimen collection, and carry out training for the medical staff of the institution.
Besides that, under the leadership and command of the State Council, close cooperation has also been carried out among the provinces. On February 7, the National Health Commission said it would take counterpart support to require other provinces to support 16 cities in Hubei Province with serious epidemic situation except Wuhan, make every effort to support Hubei Province to strengthen the treatment of patients and maintain the life safety and health of the people. The specific list of counterpart support is shown in Table 4. This counterpart support method can not only share the pressure of anti-epidemic with the strength of the whole country, solve the urgent need of Hubei Province, and curb the spread of the epidemic as soon as possible; it can also effectively integrate internal and external medical resources and rapidly improve the anti-epidemic ability of 16 cities in Hubei Province in a short time.
Table 4
| Supporting provinces | Supported cities | Supporting provinces | Supported cities |
|---|---|---|---|
| Shandong Province; Hunan Province | Huanggang City | Guangxi Province | Shiyan City |
| Chongqing Municipality City; Heilongjiang Province | Xiaogan City | Liaoning Province; Ningxia Autonomous Region | Xiangyang City |
| Jiangxi Province | Suizhou City | Yunnan Province | Xianning City |
| Jiangsu Province | Huangshi City | Shanxi Province | Xiantao City; Tianmen City; Qianjiang City |
| Guizhou Province | Erzhou City | Tianjin Municipality City | Enshi City |
| Guangdong Province; Hainan Province | Jingzhou City | Fujian Province | Yichang City |
| Zhejiang Province; Inner Mongolia Autonomous Region | Jingmen City | Hebei Province | Shennongjia Forestry District |
In addition to counterpart support, Hubei also gathered the strongest and highest level of critical care expert team in China. Top hospitals from all over the country have dispatched professional medical teams to support all cities in Hubei Province, including Peking Union Medical College Hospital, Xiangya Hospital of Central South University, Qilu Hospital of Shandong University and West China Hospital of Sichuan University, which reinforce full communication and cooperation among cross-provinces, cross-regions and cross-departments, provides sufficient talent guarantee and technical support for the control of the epidemic situation, and is also conducive to the sharing of resources and information.
Discussion
This time, China has taken rapid, decisive and accurate intervention measures in response to novel coronavirus pneumonia and dealing with public health emergencies, which not only makes great contributions to controlling the epidemic situation in China, but also ensures the health and well-being of the people of the world. The Chinese government is fully aware that this epidemic is a big challenge for the national governance system and governance capacity, so it is necessary to earnestly summarize and study the problems arising in the epidemic situation and do a good job in the prevention and control of infectious diseases and public health emergencies based on the principle of improving the system and mechanism. Specific recommendations are as follows:
Formulate and improve relevant laws and regulations in the field of public health and wildlife protection
For example, betterment the Law on the Protection of Wildlife, enhance the intensity of punishment for using and selling wildlife, introduce the Biosafety Law and accelerate the construction of national wildlife protection law and regulation system and guarantee system (13). We need carefully evaluate the law on preventing and treating communicable diseases and the law on protecting the wildlife. From the perspective of protecting people's health, safeguarding national security and maintaining long-term national stability, we need to integrate wildlife protection into the national security system, systematically plan the development of a national biosafety risk prevention and control system, and comprehensively improve the capacity of wildlife protection and public health crisis management (14).
Strengthen the construction of public health emergency management system
For example, innovate and improve the prevention and control of major epidemic situations in terms of systems and mechanisms. Measures shall be taken to improve the emergency response mechanism for major epidemic situations, establish a centralized, unified and efficient leadership and command system, and improve the ability level to respond to major public health emergencies. Strengthen the communication and cooperation mechanism among cross-provinces, cross-regions and cross-departments.
Improve and optimize the public health service system and wildlife protection system
For example, increase the investment in medical and health resources and strengthen the construction of public health teams, optimize the structure of medical personnel, and improve the training, access, use, welfare guarantee, assessment and evaluation and incentive mechanism for practicing personnel. Improve related laws and regulations on wildlife protection, strengthen market supervision, resolutely ban and severely crack down on illegal wildlife markets and trade, resolutely eliminate the habit of overeating wildlife, and control major public health risks from the source. Strengthen the protection of public health building a civic health education system, strengthen cooperation among various departments to establish correct awareness of ecological protection and public health safety.
Establish an effective synergistic mechanism for scientific research, disease control, and clinical treatment
Form institutionalized achievements and improve the prevention and control norms and emergency treatment management measures for sudden severe and extraordinarily serious epidemic situations. Improve and optimize the treatment system for major epidemic situations, establish and improve the treatment mechanism for infectious diseases with grading, stratification and diversion and other major epidemic situations, support first-line clinical technology innovation, and timely promote effective treatment plans (15).
Strengthen the international cooperation and establish a national and global public health security information network
The network should be based on the global outbreak early warning and response network (GOARN) and the healthy cities network of the World Health Organization (WHO), so as to promote international cooperation, enhance the ability to participate in global governance of public affairs and jointly respond to public crises. In line with the concept of “One Health”, health and safety collaboration among people, animals and the environment should be strengthened through establishing the information and data sharing mechanisms of multisectoral departments.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jphe.2020.03.02). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Pneumonia of unknown cause China. Available online: https://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/
- World Health Organization. Novel coronavirus (2019-nCoV) situation report-8. Available online: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200128-sitrep-8-ncov-cleared.pdf?sfvrsn=8b671ce5_2. January 28, 2020.
- US Centers for Disease Control and Prevention. 2019 Novel coronavirus, Wuhan, China: symptoms. Available online: https://www.cdc.gov/coronavirus/2019-ncov/about/symptoms.html. Published January 26, 2020. Accessed January 27, 2020.
- Riou J, Althaus CL. Pattern of early human-to-human transmission of Wuhan 2019-nCoV, bioRxiv 2020.01.23.917351. Available online: https://www.biorxiv.org/content/10.1101/2020.01.23.917351v1.full.pdf. Accessed: 27 January 2020.
- Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). Available online: https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov)
- Liu P, Chen W, Chen JP, et al. Viral Metagenomics Revealed Sendai Virus and Coronavirus Infection of Malayan Pangolins (Manis javanica). Viruses 2019;11:979. [Crossref] [PubMed]
- Matthew Wong et al. Evidence of recombination in coronaviruses implicating pangolin origins of nCoV-2019. bioRxiv, 2020.2.13 Available online: https://www.biorxiv.org/content/10.1101/2020.02.07.939207v1
- Zhou P, Yang XL, Wang XG, et al. Apneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020; [Epub ahead of print]. [Crossref]
- Ji W, Wang W, Zhao X, et al. Homologous recombination within the spike glycoprotein of the newly identified coronavirus may boost cross﹕pecies transmission from snake to human. Journal of Medical Virology 2020; [Crossref]
- The Report on 2019 Global Health Security Indicators. Available online: https://www.ghsindex.org/wp-content/uploads/2019/10/2019-Global-Health-Security-Index.pdf
- Tan ZX, Wu ST, Han XP. References and Enlightenments from the Public Health Emergency Response Systems of the United States of America and Japan—Pneumonia Epidemic Response to Novel Coronavirus pneumonia in China. Health Economics Research: 1-6[2020-02-18]. Available online: https://doi.org/
10.14055/j.cnki.33-1056/f.20200210.001 - Phelan AL, Katz R, Gostin LO. The Novel Coronavirus Originating in Wuhan, China: Challenges for Global Health Governance. JAMA 2020. [Epub ahead of print].
- The National People's Congress (NPC) has started revising the wildlife protection law. 2020-2-11. Available online: http://www.chinanews.com/
- Wang Q. Study on Prevention and Control of Novel Coronavirus Pneumonia and Improvement of National Governance Effectiveness. Health Economics Research 2020;02:1-6.
- The speech by Chairman Xi on the 12th meeting of the Central Committee for deepening reform. Available online: http://www.mod.gov.cn/shouye/2020-02/14/content_4860469.htm
Cite this article as: Xu T, Yang R. COVID-19 spread, wildlife protection and the response capacity on public health crisis: empirical research of 31 provinces and cities in China. J Public Health Emerg 2020;4:4.