
Factors associated with duration of hospital stay and complications in patients with COVID-19
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has infected millions of people globally (1). This disease was later designated coronavirus disease 2019 (COVID-19). Due to the high infectivity of SARS-CoV-2, the number of infections is surging rapidly and many countries have begun to experience outbreaks (2,3).
As the epicenter of the pandemic in the last two months, China has implemented extraordinary measures to meet the challenge of COVID-19 and an increasing number of patients are being cured. However, the prognosis of this highly infectious disease is still not well investigated. Further, no antiviral drugs with definite effects have been identified thus far (4); therefore, the main therapeutic strategy still focuses on symptomatic support. Notably, although most of the patients had nonsevere disease on admission, some of them showed poor treatment efficacy during hospitalization and developed various complications such as electrolyte disturbance, acute respiratory distress syndrome (ARDS) or multiple organ failure. Although several previous studies have introduced the epidemiological and clinical features of patients with COVID-19, they were based on relatively small numbers of patients with relatively severe conditions in the city of Wuhan, and more importantly, factors associated with clinical outcomes have not been well explored (5–7).
The present study included patients admitted to a hospital based in Guangzhou, Guangdong, China, with laboratory-confirmed COVID-19. We aimed to explore factors associated with length of hospital stay (LOS) and development of adverse complications after hospital admission. Most patients included in the present study had nonsevere disease on admission, which is similar to the real-world situation (8). This study may provide new insight into the clinical management of this disease. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/jphe-20-74).
Methods
Patients
The present study was a retrospective cohort study. A total of 285 consecutive adult patients (age ≥18 years) with a diagnosis of COVID-19 were recruited at Guangzhou Eighth People's Hospital. The admission dates ranged from January 20 to March 04, 2020. Guangzhou Eighth People’s Hospital is one of the designated hospitals for the admission of patients with COVID-19 in Guangzhou, Guangdong, China. The diagnostic criteria of COVID-19 were based on the New Coronavirus Pneumonia Prevention and Control Program (7th edition) (9). Specifically, those who met the following criteria were considered positive: (I) patients with positive SARS-CoV-2 detection by quantitative real-time reverse-transcriptase polymerase-chain-reaction (qRT-PCR) of samples from the respiratory tract; (II) patients with relevant clinical symptoms (fever or respiratory symptoms); and (III) patients with typical changes on chest radiology. Throat swab samples were collected for the detection of SARS-CoV-2 viral nucleic acids by qRT-PCR. qRT-PCR assays were performed according to the guidelines recommended by the World Health Organization (WHO) (10). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The institutional ethics board of Guangzhou Eighth People’s Hospital approved the research and granted a waiver for informed consent from the patients in this study.
Data collection
A group of experienced clinicians, epidemiologists and medical students collected information from the electronic medical record system by using a structured data collection form. The collected information included epidemiological, clinical, and outcome data. Two researchers (J.Z.Z. & R.Z.) independently reviewed and analyzed the data, and discrepancies were solved by discussion with a third researcher (F.R.L.).
Routine blood hematologic and biochemical tests to detect complete blood counts, coagulation profiles, renal and liver functioning, creatine kinase, lactate dehydrogenase (LDH), electrolytes, myocardial enzymes, C-reactive protein (CRP), and procalcitonin were carried out when necessary during hospitalization. Chest radiography or computed tomography (CT) were also performed for all inpatients. All laboratory data were obtained from the clinical laboratory of Guangzhou Eighth People's Hospital.
Definitions
Based on the recommendations by the National Health Commission (11), patients were discharged from the hospital once the following conditions were met simultaneously: (I) body temperature remained to normal for more than 3 days; (II) respiratory symptoms improved significantly; (III) acute exudative lesions were significantly improved on pulmonary imaging; and (IV) nucleic acid tests of sputum, throat swab and other respiratory samples were negative twice in a row (the sampling time was at least 24 hours apart). The degree of severity of the disease was defined according to the New Coronavirus Pneumonia Prevention and Control Program (7th edition) (9). Electrolyte disturbance was defined as an electrolyte concentration that was outside the normal range. ARDS was defined based on the Berlin definition (12). Secondary infection was diagnosed when patients showed clinical symptoms or signs of bacteremia and had positive culture results for a new pathogen in lower respiratory tract specimens or blood samples (5). Acute kidney injury (AKI) was diagnosed based on the Kidney Disease: Improving Global Outcomes (KDIGO) clinical practice guidelines (13). Myocardial damage was defined if abnormalities were observed on electrocardiography and echocardiography (5). Other complications were defined mainly according to related examinations and clinicians’ consensus after discussion.
Statistical analysis
The main analysis was performed with the data collected on admission, unless otherwise specified. Continuous variables and categorical variables were described by medians (interquartile ranges, IQRs) and frequencies (percentages, %). Differences were tested by using the chi-square test or Fisher’s exact test for categorical variables, as appropriate, and the Mann-Whitney U test for continuous variables. To compare the baseline characteristics between groups, patients were stratified based on the median LOS (<18 and ≥18 days) and whether they had developed complications during hospitalization. Binary logistic regression models were performed, with the prolonged LOS (≥18 days) as the outcome, after the exclusion of 1 patient who had died and 4 patients who were still hospitalized. Logistic models were also used to estimate the magnitude of the associations between factors and risk of developing complications. Associations were estimated in terms of per interquartile range increases for continuous variables. All the models were run with adjustment for age (age ≥60 years or not). Variables fulfilling the following criteria were not examined in the regression models: (I) between-group variables that were nonsignificant; and (II) variables with a high risk of bias (e.g., recall bias, reverse causation) such as exposure history, treatment, etc. Sample sizes varied due to missing data.
All statistical analyses were conducted using STATA, version 14 (StataCorp). All P values were 2-tailed, with statistical significance set at α of 0.05.
Results
Epidemiology and clinical features
The median age of the patients was 48 years (IQR 35–62), and 128 (44.9%) patients were male. The median time from illness onset to hospital admission was 3 days (IQR, 2–7), and the median LOS was 18 days (IQR 13–25). Of these patients, 131 (46.0%) had an LOS shorter than 18 days, 90 (31.6%) developed one or more adverse complications, 84 (29.5%) were residents of Wuhan or around; 95 (33.3%) had visited Wuhan or areas around the city and 100 (35.1%) had never been to Wuhan but had contacted with Wuhan residents or other infected patients. Overall, 88 patients (31.4%) had one or more coexisting illnesses. The most commonly self-reported symptoms on admission were fever (67.7%), followed by dry cough (56.0%), expectoration (20.7%), chills (20.4%) and fatigue (13.0%). A total of 261 (95.6%) patients initially had findings of bilateral infiltrates on radiographic imaging; 6 (2.1%) patients were classified as severe on admission. Other baseline characteristics were presented in (Table 1).
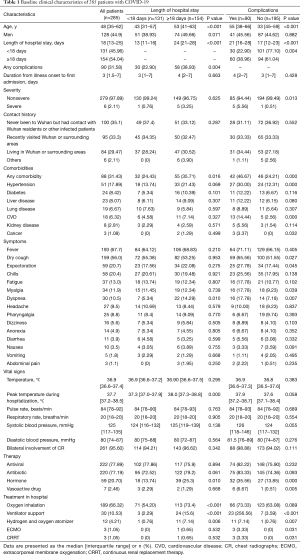
Full table
Patients with longer LOS (LOS ≥18 days) were older, had higher peak temperatures during hospitalization and were more likely to have underlying comorbidities than patients with shorter LOS (<18 days). In addition, patients with longer LOS tended to report dyspnea more often than those with shorter LOS. Patients who developed one or more complications appeared to be older, have longer LOS and have higher degrees of disease severity than patients without any complications. They were also more likely to have comorbidities, including hypertension, cardiovascular disease (CVD) and cancer; and reported dry cough, myalgia, and dyspnea more often than those without complications (Table 1).
Laboratory findings
Table 2 summarizes the laboratory findings. Many patients had the following hematologic abnormalities at presentation (only ratios ≥10% were shown): leukopenia [16.6%, white blood cell (WBC) count <3.5×109 cells/L], neutropenia (16.2%, neutrophil count <1.8×109/L), anemia (36.9%, hemoglobin level <130 g/L), lymphopenia (31.7%, lymphocyte count <1.1×109 cells/L), hypokalemia (17.3%, potassium <3.3 mmol/L), thrombocytopenia (11.2%, platelet count <125×109 cells/L), D-dimerization (83.0%, D-dimer >500 mg/L); prolonged activated partial thromboplastin time (APTT) (68.5%, >37 seconds). Levels of the following enzymes and proteins were elevated: procalcitonin (≥0.1 ng/mL) in 49.3% of patients, LDH (>243 U/L) in 23.0%, aspartate aminotransferase (AST) (>40 U/L) in 12.7%, elevated CRP levels (≥10 mg/L) in 38.4%. Analbuminaemia (albumin <40 g/L) was also observed in 49.2% of the patients. Other analytes were largely within the normal range.
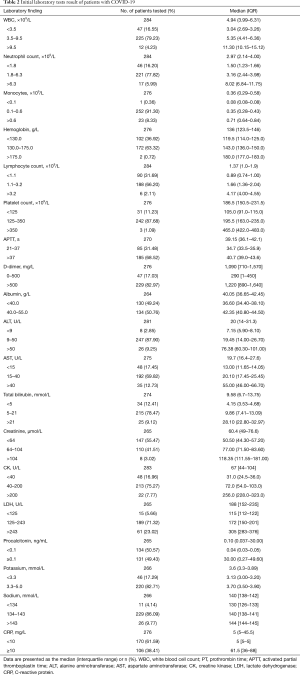
Full table
Those with LOS longer than 18 days had higher WBC counts, neutrophil counts, D-dimer, alanine aminotransferase (ALT), AST, creatinine, LDH, CRP; lower platelet counts and, sodium; and longer APTTs than those with LOS shorter than 18 days. Higher D-dimer, ALT, AST, LDH, CRP and platelet counts, albumin, and sodium were observed among those who developed complications, compared with those who did not. Serial monitoring of laboratory measures showed that during hospitalization, patients had longer LOS or those with complications generally experienced significant increases in the incidence of abnormal blood biochemical parameters, compared with those with shorter LOS or those who had no complications (Table S1).
Clinical courses and outcomes
During hospitalization, all patients received either antibiotic therapy, antiviral therapy, hormonal therapy, vasoactive drug therapy, or a combination of the above based on clinical experience. The median time from admission to the development of any complication was 13 days (IRQ 8–21). Twenty (7.0%) patients were admitted to the intensive care unit (ICU), and 3 (1.1%) patients received extracorporeal membrane oxygenation (ECMO) or continuous renal replacement therapy (CRRT). Eventually, 280 (98.3%) patients were discharged from the hospital and 1 (0.4%) patient died. According to our case definition, 90 (31.6%) patients developed complications during their hospital stay. Electrolyte disturbance was the most common complication (15.1%), followed by liver damage (11.9%), secondary infection (5.3%), and AKI (3.9%). Other concurrent medical conditions included respiratory failure, ARDS, disseminated intravascular coagulation (DIC), shock, myocardial damage, and atrial fibrillation, etc. (Table S2). During hospitalization, many symptoms, such as anorexia, dyspnea, nausea became increasingly prevalent, affecting up to 41.4%, 34.7%, and 25.3% of the patients, respectively (Table S3).
Associations between factors and LOS and adverse complications
Those with longer LOS presented with more complications than those with shorter LOS. Additionally, patients who developed complications during hospitalization tended to have longer LOS than those without complications. We used logistic regression to explore the associations of various factors with LOS and complications. Age-adjusted models revealed that the following factors were linked to both a longer LOS and complications: older age (OR =2.00, 95% CI, 1.18–3.40 for LOS; OR =2.24, 95% CI, 1.32–3.80 for complication), relatively high neutrophil counts (OR =1.60, 95% CI, 1.18–2.17; OR =1.30, 95% CI, 1.03–1.64), CRP (OR =1.49, 95% CI, 1.09–2.05; OR =1.70, 95% CI, 1.25–1.31) and D-dimer (OR =1.37, 95% CI, 1.04–1.81; OR =1.25, 95% CI, 1.02–1.55). Factors such as WBC (OR =1.44; 95% CI, 1.07–1.95) and APTT (OR =1.57; 95% CI, 1.12–2.20) were positively associated with the longer LOS but not with complications. On the other hand, comorbidities (OR =2.33; 95% CI, 1.33–4.10), elevated ALT (OR =1.25; 95% CI, 1.05–1.50), elevated AST (OR =1.49; 95% CI, 1.23–1.82) and elevated LDH (OR =1.39; 95% CI, 1.08–1.79) were significantly associated with the risk of complications but not the longer LOS (Table 3).
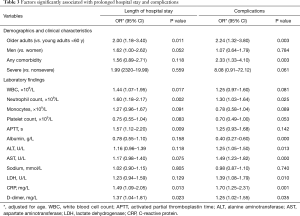
Full table
Discussion
In this retrospective cohort study, we reported the characteristics and factors associated with LOS and complications during hospitalization in patients with COVID-19 at a designated hospital in Guangzhou, Guangdong, China. In our study, a large proportion of patients had abnormal clinical conditions on admission, but most of the included patients had a favorable prognosis. We found that advanced age; relatively high neutrophil counts, CRP and D-dimer levels were associated with both prolonged LOS and elevated risk of adverse complications.
During the outbreak of COVID-19, medical resources have been exhausted in many countries. Understanding hospital LOS and factors related to LOS may provide important information to inform clinicians about patient selection, the development of strategies to reduce hospital LOS, and how to ultimately reduce resource utilization. Our study recorded a longer LOS (18 days) than some other studies in Wuhan (14,15), where the average LOS for COVID-19 patients was nearly 12 days. These differences may be because study populations in Wuhan were not representative of all cases diagnosed and treated in China. Many patients may have been transferred late in their illness to hospitals during the initial outbreak. Additionally, it is possible that a large proportion of patients in the above studies were still hospitalized at the time of publication and the shortage of medical resources led to some patients being discharged in advance to make room the new case.
So far, there have been no antiviral drugs with definite effects identified, and thus the main therapeutic strategy for COVID-19 still focuses on symptomatic support. Unlike previous studies that recorded many cases of ARDS and respiratory failure (15,16), the most common complications in this study were electrolyte disturbances, followed by liver damage, secondary infection, AKI. Electrolyte disturbances, such as hypokalemia can potentially be fatal but is amenable by relatively simple interventions. The frequent observance of electrolyte disturbances has not been reported in previous studies of COVID-19, but it is in line with the results of a few studies of Ebola patients (17). However, as electrolyte disturbance complication could be commonly observed in critically ill patients hospitalized for long periods (18), we could hardly confirm it a distinctive characteristic of patients with COVID-19. Additionally, renal dysfunction, pancreatitis and sepsis could contribute to this disorder (19). Multiple organ injury is common in patients with COVID-19. Our data showed that biomarkers of impaired organ function such as ALT, AST and LDH were elevated on admission in those patients with complications. The exact cause of organ injury remains unknown, but both the hyperinflammation and viral evasion are likely involved (20,21).
In the present study, older age appeared to be associated with prolonged hospitalization and an increased risk of developing complications. Indeed, it is well recognized that older age is an important predictor of adverse outcomes, and previous studies of severe acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS) and COVID-19 confirmed these findings (15,22,23). Older age may be a proxy for a deficiency in the control of viral replication and less-robust immune responses (24), potentially leading to adverse clinical outcomes (25). Prior studies have also found that comorbid diseases were the most common reasons for continued hospitalization among patients with community-acquired pneumonia (26). The poor health status of those with comorbid illnesses may lead to complications and additional treatment, leading to prolonged hospitalization.
The pathogenesis of highly pathogenic SARS-CoV-2 is still not completely understood, but virally driven hyperinflammation are thought to play important roles in disease severity (27,28). In this study, we found that increased levels of several inflammation-related factors, such as neutrophil and CRP were associated with adverse outcomes. Neutrophils are the main source of chemokines and cytokines. It has been reported that increased levels of neutrophilia were common in both the peripheral blood and lungs of patients with SARS and MERS (29–31). These abnormalities suggest that increased levels of neutrophilia may be a common characteristics of coronavirus infection. The monitor on this index should be intensified during hospitalization since various of infections are commonly related to this condition and may consequently lead to poor outcome. Moreover, clinical analysis on it should be more prudent and comprehensive. (e.g., taking the patients’ status of use of corticosteroids into account owing to its confounding effects on neutrophilia). CRP is an acute-phase protein that increases with infection during virally driven hyperinflammation. A previous study demonstrated that the detection rate of respiratory viruses was strongly associated with CRP levels (32). As the host inflammatory response can be measured by CRP levels, CRP could also be used in clinical practice to guide viral testing and directed antiviral therapy where available (33).
Elevated D-dimer, as a degradation product of fibrinogen breakdown, could be a marker of impaired coagulation function. Therefore, the higher risk of thromboembolic events (demonstrated by high D-dimer levels and APTT) in patients with COVID-19 could not be ignored. Further evidence is urgently needed regarding the coagulation pathways that related to the SARS-CoV-2 infection. It’s notable that secondary infection was a common complication among patients in current cohort. The rate is similar to those in the previous report (5). One possible explanation is that the amount or time of antibiotics is excessive, which may lead to the imbalance of normal flora in human body and in turn secondary infection. Furthermore, invasive mechanical ventilation may increase the risk of secondary infection which deserved more clinical attention.
Strengths and limitations
This study analyzed a relatively large sample size to describe the characteristics and determinants of LOS and complications in a cohort of patients with COVID-19 at a designated hospital outside of Wuhan. The results from our study should be interpreted with caution because of potential bias and residual confounding due to its retrospective nature. Also, data were collected from case records and thus not systematic. Selection bias should also be considered when exploring factors that are related to clinical outcomes.
Conclusions
During the COVID-19 pandemic, the priority for clinical practices is to identify people with a high risk of progressing to poor clinical outcomes. We found that advanced age, higher levels of neutrophil counts, D-dimer and CRP were potential predictors for both longer LOS and elevated risk of adverse complications.
Acknowledgments
Funding: This work was sponsored by Open Project of Guangdong Provincial Key Laboratory of Tropical Disease Research (KLTDR2020003).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/jphe-20-74
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jphe-20-74
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jphe-20-74). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The institutional ethics board of Guangzhou Eighth People’s Hospital approved the research and granted a waiver for informed consent from the patients in this study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zhu N, Zhang D, Wang W, et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med 2020;382:727-33. [Crossref] [PubMed]
- Kandel N, Chungong S, Omaar A, et al. Health security capacities in the context of COVID-19 outbreak: an analysis of International Health Regulations annual report data from 182 countries. Lancet 2020;395:1047-53. [Crossref] [PubMed]
- Lai CC, Shih TP, Ko WC, et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. Int J Antimicrob Agents 2020;55:105924. [Crossref] [PubMed]
- Cao B, Wang Y, Wen D, et al. A Trial of Lopinavir-Ritonavir in Adults Hospitalized with Severe Covid-19. N Engl J Med 2020;382:1787-99. [Crossref] [PubMed]
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497-506. [Crossref] [PubMed]
- Chang D, Lin M, Wei L, et al. Epidemiologic and Clinical Characteristics of Novel Coronavirus Infections Involving 13 Patients Outside Wuhan, China. JAMA 2020;323:1092-3. [Crossref] [PubMed]
- Zhang JJ, Dong X, Cao YY, et al. Clinical characteristics of 140 patients infected by SARS-CoV-2 in Wuhan, China. Allergy 2020;75:1730-41. [Crossref] [PubMed]
- Niforatos JD, Melnick E, Faust J. Covid-19 fatality is likely overestimated. BMJ 2020;368:m1113. [Crossref] [PubMed]
- “National Health Commission of China.” New coronavirus pneumonia prevention and control program (7th edition) [Internet] 2020 [cited 2020 Mar 3]. Available online: http://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989/files/ce3e6945832a438eaae415350a8ce964.pdf
- “World Health Organization.” Laboratory testing for 2019 novel coronavirus (2019-nCoV) in suspected human cases [Internet]. [cited 2020 Mar 12]. Available online: https://www.who.int/publications-detail/laboratory-testing-for-2019-novel-coronavirus-in-suspected-human-cases-20200117
- “National Health Commission of China.” New Coronavirus Pneumonia Prevention and Control Program (6th edition) [Internet]. [cited 2020 Feb 18]. Available online: http://www.nhc.gov.cn/jkj/s3577/202003/4856d5b0458141fa9f376853224d41d7.shtml
- Antonelli M. Acute respiratory distress syndrome. The Berlin Definition, Berlin, 2012.
- Khwaja A. KDIGO Clinical Practice Guidelines for Acute Kidney Injury. Nephron Clin Pract 2012;120:c179-84. [PubMed]
- Wang D, Hu B, Hu C, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China. JAMA 2020;323:1061-9. [Crossref] [PubMed]
- Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study 2020,395:1054-62.
- Wu C, Chen X, Cai Y, et al. Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern Med 2020;180:934-43. [Crossref] [PubMed]
- van Griensven J, Bah E, Haba N, et al. Electrolyte and Metabolic Disturbances in Ebola Patients during a Clinical Trial, Guinea, 2015. Emerg Infect Dis 2016. [Crossref] [PubMed]
- Lindner G, Kneidinger N, Holzinger U, et al. Tonicity Balance in Patients With Hypernatremia Acquired in the Intensive Care Unit. Am J Kidney Dis 2009;54:674-9. [Crossref] [PubMed]
- Collage RD, Howell G, Zhang X, et al. Calcium Supplementation During Sepsis Exacerbates Organ Failure and Mortality via Calcium/Calmodulin-Dependent Protein Kinase Kinase Signaling. Crit Care Med 2013;41:e352-60. [Crossref] [PubMed]
- Hotchkiss RS, Moldawer L, Opal S, et al. Sepsis and septic shock. Nat Rev Dis Prim 2016;2:16045. [Crossref] [PubMed]
- Lelubre C, Vincent JL. Mechanisms and treatment of organ failure in sepsis. Nat Rev Nephrol 2018;14:417-27. [Crossref] [PubMed]
- Choi KW, Chau T, Tsang O, et al. Outcomes and Prognostic Factors in 267 Patients with Severe Acute Respiratory Syndrome in Hong Kong. Ann Intern Med 2003;139:715-23. [Crossref] [PubMed]
- Hong KH, Choi JP, Hong SH, et al. Predictors of mortality in Middle East respiratory syndrome (MERS). Thorax 2018;73:286-89. [Crossref] [PubMed]
- Busse PJ, Mathur S. Age-related changes in immune function: Effect on airway inflammation. J Allergy Clin Immunol 2010;126:690-9. [Crossref] [PubMed]
- Opal SM, Girard TD, Ely EW. The Immunopathogenesis of Sepsis in Elderly Patients. Clin Infect Dis 2005;41:S504-12. [Crossref] [PubMed]
- Menéndez R, Ferrando D, Vallés JM, et al. Initial risk class and length of hospital stay in community-acquired pneumonia. Eur Respir J 2001;18:151-6. [Crossref] [PubMed]
- Channappanavar R, Perlman S. Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology. Semin Immunopathol 2017;39:529-39. [Crossref] [PubMed]
- D’Antiga L. Coronaviruses and immunosuppressed patients. The facts during the third epidemic. Liver Transpl 2020;26:832-4. [Crossref] [PubMed]
- Min CK, Cheon S, Ha NY, et al. Comparative and kinetic analysis of viral shedding and immunological responses in MERS patients representing a broad spectrum of disease severity. Sci Rep 2016;6:25359. [Crossref] [PubMed]
- Ng DL, Al Hosani F, Keating MK, et al. Clinicopathologic, Immunohistochemical, and Ultrastructural Findings of a Fatal Case of Middle East Respiratory Syndrome Coronavirus Infection in the United Arab Emirates, April 2014. Am J Pathol 2016;186:652-8. [Crossref] [PubMed]
- Kim ES, Choe P, Park W, et al. Clinical Progression and Cytokine Profiles of Middle East Respiratory Syndrome Coronavirus Infection. J Korean Med Sci 2016;31:1717-25. [Crossref] [PubMed]
- Clark TW, Medina MJ, Batham S, et al. C-reactive protein level and microbial aetiology in patients hospitalised with acute exacerbation of COPD. Eur Respir J 2015;45:76-86. [Crossref] [PubMed]
- Chalmers JD, Singanayagam A, Hill A. C-reactive Protein Is an Independent Predictor of Severity in Community-acquired Pneumonia: What Does It Add to? Am J Med 2008;121:219-25. Reply. [Crossref] [PubMed]
Cite this article as: Chen FJ, Li FR, Zheng JZ, Zhou R, Liu HM, Wu KY, Zhang B, Dong H, Lu JY, Lei CL, Wu XB. Factors associated with duration of hospital stay and complications in patients with COVID-19. J Public Health Emerg 2021;5:6.


