
Problems related with the use the statins in primary health care, Cali-Colombia
Introduction
Dyslipidemia is a metabolic disorder with significant prevalence worldwide. In Colombia, an increase in dyslipidemia prevalence of almost 3% per year has been determined (1). Dyslipidaemia increases the risk of morbidity and death from cardiovascular diseases (CVD) including ischemic heart disease, which is among the leading cause of death worldwide (1). The therapeutic interventions for hypercholesterolemia should be aimed at treating cardiovascular risks (CVR) and not exclusively cholesterol (2). The Framingham risk score (FRS) is the most widely used CVR prediction tool, prevising the risk of incident CVD events over the subsequent 10 years (3).
Obesity, is probably the main cause of the metabolic syndrome, and is related with other CVR factors such as insulin resistance, type 2 diabetes mellitus (DM), high blood pressure (HBP), obstructive sleep apnea syndrome, non-alcoholic fatty liver disease and dyslipidemia (4). The effectiveness of high adherence to healthy habits such as dietary changes and exercise on hyperlipidemia has been clearly reported in the literature. However, many counseled patients poorly adhere to a healthy nutritional plan (5).
Treatment of obesity-associated dyslipidemia should be focused on lifestyle changes including weight loss, physical exercise and a healthy diet (4). However, pharmacological therapy can be initiated and be effective if lifestyle changes are insufficient or with the presence of other CVR factors (DM, HBP) or CVD. Statins have been described to be the primary lipid lowering drugs with effective reductions in LDL and remnant cholesterol levels (4,6), and are recommended in the treatment for secondary CVR prevention in patients with ischemic CV disease of atherosclerotic origin. However, there is a substantial gap between current guidelines recommendations and clinical practice (6,7).
One way to ensure the clinical objective of optimal cholesterol levels is to follow up with pharmacotherapy with patients who have an indication for statins, aimed at detecting drug-related problems (DRP), establishing a causal relationship with their risk factors and propose intervention strategies appropriate to their needs. A DRP can be defined as a health problem related to pharmacotherapy and that which interferes or may interfere with expected health outcomes in the patient (8).
During an internal audit conducted in the primary health centre Comfandi Network in 2016, it was reported that there were patients with a clinical diagnosis of dyslipidemia according to the Institution’s Clinical Practice Guideline (CPG) who had no prescription of statins and a number of them received doses below what was recommended in this guideline. In addition to dyslipidemia, another part of the population that could be greatly benefited from the use of statins and healthy lifestyle habits are patients with other CVR factors, such as patients diagnosed with hypertension and/or diabetes. For this reason, in the present study, hypertensive and diabetic patients belonging to the chronic program were also included.
There are no recent studies in Colombia on DRP with statins; no studies were identified that analysed both DRP and non-pharmacological treatment compliance. DRPs have an impact on patient health (9) and healthcare costs (10), and Colombia is a middle income country with certain limitations in the healthcare services (11). Recent data shows that 35.6% of the chronic patients in urgent service presented at least one negative outcome associated with medication (NOM), mainly linked to safety (12) and 43 NOMs were identified in hospitalized patients (13). Therefore, it is essential to identify the DRPs and establish intervention strategies.
For all the above, the objective of this study was to determine DRP with the use of statins in dyslipidemic, hypertensive and diabetic patients as well as with other factors like adherence to diet/exercise plan and CVD risk.
We present the following article in accordance with the STROBE reporting checklist and MDAR checklist (available at http://dx.doi.org/10.21037/jphe-20-63).
Methods
A retrospective and descriptive study was carried out in a primary health care (PHC) centre, which has a comprehensive care Chronic Unit Program Integral (UPI), which is focused on the protection of renal function of patients with deterioration-related diseases of the kidney. Patients over 18 years of age who attended a consultation at the UPI between January 2016 and September 2017 treated at the PHC Prado, who presented one or more of the following diseases: HBP, DM and/or dyslipidemia were enrolled. Patients who were not active in the UPI program in July 2017 were excluded.
The sample size was estimated based on the total number of patients belonging to the Chronic UPI program who were active as of July 2017 (11,626 patients). From this population and considering that, the prevalence of occurrence of DRP in chronic UPI patients was 57.93% in a previous study in PHC Prado (unpublished), and using a 95% confidence level and an error of 7%, the sample size was calculated in 132 patients.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Both ethics committees, the PHC Comfandi and the Icesi University (Approval Act number 124 of June 14, 2017), approved the study, and the privacy of the individual was protected by respecting the confidentiality of each patient's data, which were used exclusively for research purposes. Informed consent was not required from the patients, as there was no contact with them, only access to their medical records, approved by the PHC. Patient information was obtained through computerized medical records provided by the PHC centre.
Independent variables
The information obtained contained the following independent variables such as demographic data (age, sex), comorbidities (yes or no for each patient diagnosis), history of cardiovascular events, Framingham 10-year risk score (FRS) of CVD (value reported in clinical record). FRS level was classified as low (FRS <10%), moderate (FRS between 10% and 19%) and high (FRS >20%), according to the CPG of PHC centre. Other variables were, history of CV laboratory tests (lipid profile), prescribed medications and diet/exercise compliance (Did you follow a specific diet and/or exercise program, recommended by a health expert, frequently and consistently during the last year? Answer: Yes, No). Factors of dyslipidemia (yes or no for each factor: obesity, hypothyroidism, metabolic syndrome, alcohol abuse and smoker). Statin indication for dyslipidemia (it was recorded whether the treatment was for primary prevention or secondary prevention, according to the CPG of PHC centre. Dosage was recorded for each medication).
DRP identification: dependent variable
DRP identification information was collected systematically by pharmacists, using the classification of Cipolle et al. (8). DRP classification consists of four categories: Indication, effectiveness, security and compliance. DRP indication was defined when the patient needed additional drug therapy (DRP 1) or had an unnecessary drug (DRP 2) according to their medical condition. The effectiveness of DRP was defined when the patient had a state of health for which he was taking the wrong medication (DRP 3) or the patient had a medical condition for which the quantity of the correct drug is being taken is insufficient (DRP 4). The security of DRP was defined when, the patient had a state of health resulting from suffering an adverse drug reaction (DRP 5) or the patient had a state of health for which he was taking too much of a correct medication. DRP compliance (DRP 7) was defined when the patient had a state of health resulting from not taking an indicated medication.
In order to analyse the existence of any DRP, it was necessary to review each patient's diagnosed disease, each prescribed medication, their dosage, main adverse reactions of statins and interactions with other drugs. It was also necessary to analyse the results of the laboratory tests (cholesterol, LDL, HDL, triglycerides). The DRP variable was managed as dichotomous, (Yes or No) in the presence or absence of each DRP (DRP 1–DRP 7); a patient could have more than one DRP.
Statistical analysis
A descriptive analysis of the variables studied was performed. For the DRP, the category and medications involved were described, summarized in frequency tables. The association between some variables with the appearance of DRP was analysed, determining the odds ratio of a 95% CI. The regression analysis was adjusted for age, gender, the number of prescribed medications, the number of underlying diseases, the history of cardiovascular events, FRS, diet and exercise compliance. In light of the possibility of investigator bias (AMT) in the identification of DRPs, a second assessor (EPR) reviewed all the medical records of the included patients and confirmed the presence or absence of DRPs with their respective category. The analyses were performed in Stata® 13.1.
Results
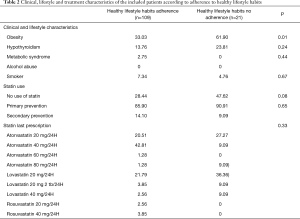
One hundred and thirty-two patients participated in this study, 54% of them were women. Information on adherence to healthy habits (diet and exercise) was obtained from 130 patients. 21 patients (16.15%) reported no compliance with diet/exercise. Table 1 presents demographic and clinical characteristics of patients according to their adherence on a healthy diet/exercise plan. There were no differences between the groups, except in sex and FRS score (P=0.03). The average age was approximately 60 years. The majority of patients were hypertensive (88%). About 28% had dyslipidemia in conjunction with HBP and/or DM. The mean of FRS was lower in those who adhered to a diet/exercise plan with statistically significant differences (P=0.03). About 35% and 43% of the patients had prescribed five or more medications in those who adhered to a healthy diet and exercise and in those who did not respectively.

Full table
The main risk factor for dyslipidemia was obesity, with significant difference between patients that followed healthy habits and those who did not (P=0.01). Thirty-one patients were not prescribed statin treatment and the majority of those who were prescribed statins were for primary prevention. Lovastatin 20 mg was the statin drug therapy that was prescribed the most, followed by atorvastatin 20 mg (Table 2).
Full table
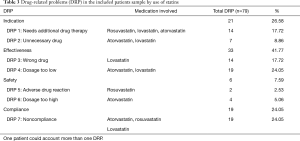
A total of 79 DRPs were associated with the use of statins among the 132 patients. At least one DRP was detected in 60 patients (45%), with a mean number 1.32±0.57 per patient. Table 3 shows DRPs and the medications that were involved. DRP in the effectiveness category was identified among the majority of the patients (42%), with sub-dosing adherence being the most frequent case. The DRP by indication category was the 27%, mainly for needing additional drug therapy. A total of 24% of DRPs reported non-compliance (DRP 7), and of these four did not adhere to healthy habits. The security DRP category was shown among 8% of the patients. Atorvastatin was implicated in all categories of DRPs.
Full table
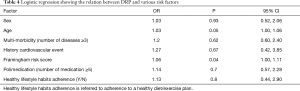
Table 4 shows the factors that were associated with the appearance of DRPs. Advanced age and high level of CVD risk according to FRS were the factors positively associated with the presence of DRP [OR, 95% CI: 1.03 (1.00, 1.06) and 1.06 (1.00, 1.11) respectively]. Multi-morbidity, poly-medication and higher adherence to healthier habits were not related with the appearance of DRPs.
Full table
Discussion
This study evaluated the association DRPs with the use of statins and among other factors, the effect of adherence to healthy habits and high CVD risk level using the FRS score in dyslipidemic, hypertensive and/or diabetic patients belonging to the Chronic UPI program in the period from January 2016 to September 2017. In the univariate analysis, we found in our sample that adherence to healthy habits were related with less CVR as defined by FRS score, and no adherence was related with higher obesity prevalence. We also found that main DRPs were effectiveness and poor indication. Additionally, we found that the adjusted analysis revealed a positive relation among DRPs, FRS score and advanced age, while there was no relation of DRs with healthy habits. With a healthcare system under crisis (10), findings like these call for attention in DRPs of statins treatment and enhancement in primary care services and patient management in Colombia.
Obesity was a risk factor found in this population related to no adherence to healthy lifestyle habits, a fact that is well-known in the literature. Treatment of obesity-associated with dyslipidemia should be focused on lifestyle changes including weight loss, physical exercise and a healthy diet (4). However, not all patients in Colombia adhere to healthy lifestyle guidelines, as reported in the present study. Only 16% of patients adhere to a healthy life-style as was recommended by their physician (diet/exercise). Results from a recent meta-analysis show that intense physical exercise increases HDL-cholesterol levels, and decreases total and triglyceride cholesterol (14). A study done on severely obese population revealed it to be associated with higher prevalence of hypertension, systolic and diastolic blood pressure, C-reactive protein, waist circumference, body fat% and family history of heart diseases, enhancing the risk for the occurrence of CVD (15). In addition, our study found that there was no relationship between healthy lifestyle and DRP.
In a study done in PHC in patients with UPI chronic, it was identified that the pharmacological adherence ranged from 20% to 91% depending on the test used, and the non-pharmacological adherence was 59% (16). However, unlike the current study, the authors used pharmacological adherence tests and asked the patient for the adherence to lifestyle recommendations (exercise, diet) and in the present study, the data was obtained from the clinical record of the patients.
In the current study, 19 DRPs (24%) were identified for non-compliance with statins. Patients with chronic diseases like HBP, DM and dyslipidemia have cardiovascular or cerebrovascular risk and usually follow a non-pharmacological and pharmacological treatment as primary or secondary prevention. However, it is difficult for patients to adhere with this kind of treatment with the consequences that may present. A systematic literature review and meta-analysis (17) showed that a considerable proportion of all CVD events could be attributed to poor adherence to cardiovascular medications and that the level of optimal adherence confers a significant inverse association with subsequent adverse outcomes.
The FRS was related to higher DRP presence among patients; FRS is the most applicable method for predicting the person’s chance of developing CVD in 10 years (18). It is important to remark that in the current study, the FRS was significantly higher in patients who did not adhere with a healthy diet/exercise. The 72.7% of the population studied had a low FRS, 19.7% had a moderate FRS and only 7.6% showed a FRS high. These findings show that patients of high CV risk are not adhering to healthy habits as primary preventive and non-pharmacological measures, and are also having higher pharmacological treatment related problems. These results call for enhancement of education strategies in vascular health and pharmacological use (especially statins) (19). Therefore, it is necessary to continue promoting healthy lifestyles in patients with CVR. For example, yoga-based intervention showed a significant reduction in FRS, and a positive correlation between reduction in FRS and serum total cholesterol (20).
Another factor associated with the presence of DRP in the current study was advanced age. This result coincides with a previous study (21), in which they identified that the average DRP per patient was higher in older age groups. However, data published in another study (22) reported no association between age and DRP. The elderly population is at greater risk for medication-related problems as a result of age-related physiological changes (example pharmacokinetic, and pharmacodynamics changes), the presence of multiple chronic diseases (like CVD) and conditions, and the types and numbers of prescription and non-prescription medications they consume (23). There is controversial data regarding the indication of statin in elderly patients. A meta-analysis (24) about the usefulness of treatment of hypercholesterolemia with statins for primary prevention in patients older than 75 Years concluded that there is a benefit of statin treatment for primary prevention in persons >75 years of age. In our study of the 90 patients with a statin indication, 17 were over 75 years of age, and of these, 82% were indicated for primary prevention. The main concerns of patients about statin use are the side effects (25,26), and interactions (25).
Some patients doubted the necessity of, or lacked knowledge about the efficacy of statins, or they had encountered practical problems regarding information about statins (26); these concerns are related with non-adherence (26). The aforementioned could be used by stakeholders in Colombia, whose populations is ageing fast, to plan, develop, and implement ageing-centred programmes that will take into account older adults pharmacological adherence problems. Regarding the prescribed medications, it was shown that 43.2% of the patients are poly-medicated, which constitutes a high proportion of patients who are at risk of not adhering to statin treatment (and in general to any therapeutic group). In other studies, a direct relationship has been established between being a noncompliant and polypharmacy, so that therapeutic non-compliance affected 30–50% of elderly patients (over 65 years of age) and in poly-pharmaceuticals it reached up to 47.6% (27). In patients with CVD, this association has been shown (22) before. New findings showed that patients with polypharmacy (11 or more medications) were almost 2 times more likely to experience an MRP than those taking fewer medications (28), however in our study we found no significant differences between poly-medicated patients and the presence of DRP, a finding that further longitudinal studies will need to investigate.
In total, 79 DRPs related to use of statins were found. Effectiveness DRP category was the most common (42%) among all DRPs. Our results are much higher in comparison with previous publications in this topic (29). In our study, it was found that in 18% of the cases, the patient had an inadequate statin prescribed (DRP 3). This was due to the prescription of different doses among statins, as supported by the literature (30). It was also found that in 24% of the cases, the patient presented an adequate underdosing (DRP 4) of the statin—a result that was in the opposite direction of another study in which it was revealed that the excessive dosage (30.4%) of statin was the second cause of DRP (31). DRPs for too low dosage (DRP 4) and patients’ needs of additional drug therapy (DRP 1) could be related to the attitude of the physician and with clinical inertia. One the main causes of uncontrolled CV risk factors are therapeutic noncompliance and clinical inertia. These causes have been shown in HBP (32,33), DM (34,35) and dyslipidemia (36-38). A recently published study in Latin America revealed that dyslipidemia treatment in patients with type 2 DM was delayed despite its known deleterious effect on atherosclerosis development and β-cell mass/function (35).
In the light of the results of this study, the non-adherence to pharmacology and lifestyle of some of the patients studied is reflected, as well as the therapeutic inertia on the part of the clinicians. The identification of these causes of DRP could guide health managers and professionals in the future for the proposal of strategies to prevent these two major problems in the achievement of therapeutic objectives. Therefore, we suggest that follow-up programs be carried out on patients with a higher risk of presenting DRP, such as older patients and those with medium or high FRS. It is also essential to promote more training for doctors to avoid therapeutic inertia.
Strengths and limitations
The findings of this study might be interpreted considering both strengths and limitations. There are few studies of DRP associated with the use of statins in Colombia. Additionally, non-adherence to lifestyle habits and the impact on obesity, dyslipidemia and DRP, as well as the factors associated with DRP were analyzed. For each DRP identified, an intervention strategy was proposed, which was passed on to the medical directors of the PHC so that they could take the appropriate actions. With the results of this study, the role of the pharmacist in primary care is highlighted—since in Colombia, the pharmacist’s assistance in all the PHCs is not established. The study was made using real world evidence, and this fact to promote the use of this source to analyze other therapeutic groups for example for HBP, DM or other chronic medicines.
One of the limitations of the study was its local character; it is impossible to generalize the findings/the data/ the records of our primary care center to that of others. Additionally, it is worth mentioning that the study was subject to the limitations of the information recorded in the medical records, so the detected DRPs may be undervalued. For instance, the doctor stated that on some occasions, the patient would present discomfort from taking statins. However, this does not patently suggest an adverse drug reaction, so it would have been better to have had direct contact with the patient for the identification of the DRP.
Conclusions
A high proportion of patients with DRP in statins were identified, mainly due to inadequate dosage of statin, therapeutic non-compliance and need for a statin prescription. Advanced age and high CVR (as defined by Framingham score) were related to the presence of DRPs in statins; however, there was no association with adherence to healthy lifestyle habits (exercise/diet).
Acknowledgments
We thank the primary health care centre Comfandi.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist and MDAR checklist. Available at http://dx.doi.org/10.21037/jphe-20-63
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jphe-20-63
Peer Review File: Available at http://dx.doi.org/10.21037/jphe-20-63
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jphe-20-63). Dr. Tyrovolas serves as an unpaid editorial board member of Journal of Public Health and Emergency from May 2020 to April 2022. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Both ethics committees, the PHC Comfandi and the Icesi University (Approval Act number 124 of June 14, 2017), approved the study, and the privacy of the individual was protected by respecting the confidentiality of each patient's data, which were used exclusively for research purposes. Informed consent was not required from the patients, as there was no contact with them, only access to their medical records, approved by the PHC. Patient information was obtained through computerized medical records provided by the PHC centre.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Machado-Alba JE, Machado-Duque ME. Cardiovascular risk factors prevalence among patients with dyslipidemia in Colombia. Rev Peru Med Exp Salud Publica 2013;30:205-11.
- Pallarés-Carratalá V, Pascual-Pérez R. Non-compliance and therapeutic inertia: two unanswered questions in clinical practice. Curr Med Res Opin 2014;30:839-40. [Crossref] [PubMed]
- D'Agostino RB Sr, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation 2008;117:743-53. [Crossref] [PubMed]
- Klop B, Elte JW, Cabezas MC. Dyslipidemia in obesity: mechanisms and potential targets. Nutrients 2013;5:1218-40. [Crossref] [PubMed]
- Kelly RB. Diet and Exercise in the Management of Hyperlipidemia. Am Fam Physician 2010;81:1097-102. [PubMed]
- Viscogliosi G, Donfrancesco C, Lo Noce C, et al. Prevalence and Correlates of Statin Underuse for Secondary Prevention of Cardiovascular Disease in Older Adults 65-79 Years of Age: The Italian Health Examination Survey 2008-2012. Rejuvenation Res 2020;23:394-400. [Crossref] [PubMed]
- Umapathi KK, Thavamani A. Statin Prescription Rates in Children With Severe Dyslipidemia in the United States. Am J Cardiol 2020;131:139-40. [Crossref] [PubMed]
- Cipolle R, Strand LMP. Drug therapy problems. In: Cipolle R, Strand L, Morley P. editors. Pharmaceutical Care Practice. The Clinician’s Guide. 2nd ed. New York: McGraw-Hill, 2004.
- Wu TY, Jen MH, Bottle A, et al. Ten-year trends in hospital admissions for adverse drug reactions in England 1999-2009. J R Soc Med 2010;103:239-50. [Crossref] [PubMed]
- Watanabe JH, McInnis T, Hirsch JD. Cost of Prescription Drug-Related Morbidity and Mortality. Ann Pharmacother 2018;52:829-37. [Crossref] [PubMed]
- Webster PC. Health in Colombia: a system in crisis. CMAJ 2012;184:E289-90. [Crossref] [PubMed]
- Parody Rua E, Montaño Holguin MA. Evaluación de resultados negativos de la medicación en el servicio de urgencias de un hospital, Cali, Colombia: Estudio transversal. Pharmaceutical Care Españ 2018;20:371-88.
- Hernández O. Seguimiento farmacoterapéutico en pacientes del servicio de medicina interna de un hospital universitario de alta complejidad. Revista Colombiana de Ciencias de la Salu 2012;1:26-33.
- Canalizo E, Salas J, Jara R, Viniegra A. Diagnóstico y tratamiento de las dislipidemias. Rev Med Inst Mex Seguro So 2013;51:700-9.
- Santos ASAC, Rodrigues APS, Rosa LPS, et al. Cardiometabolic risk factors and Framingham Risk Score in severely obese patients: Baseline data from DieTBra trial. Nutr Metab Cardiovasc Dis 2020;30:474-82. [Crossref] [PubMed]
- Parody-Rúa E, Vásquez-Vera A. Prevalencia y factores asociados a la adherencia terapéutica en pacientes de un programa integral de crónicos en un centro de atención primaria de Cali: comparación de diferentes test de adherencia. Pharmaceutical Care Españ 2019;21:23-40.
- Chowdhury R, Khan H, Heydon E, et al. Adherence to cardiovascular therapy: a meta-analysis of prevalence and clinical consequences. Eur Heart J 2013;34:2940-8. [Crossref] [PubMed]
- Wilson PW, D'Agostino RB, Levy D, et al. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837-47. [Crossref] [PubMed]
- Cubillo EI 4th, Rosenfeld DM, Hagstrom SG, et al. Patient understanding of the importance of statin use in the perioperative period. J Cardiothorac Vasc Anesth 2015;29:670-7. [Crossref] [PubMed]
- Yadav R, Yadav RK, Sarvottam K, et al. Framingham Risk Score and Estimated 10-Year Cardiovascular Disease Risk Reduction by a Short-Term Yoga-Based LifeStyle Intervention. J Altern Complement Med 2017;23:730-7. [Crossref] [PubMed]
- Lee JS, Yang J, Stockl KM, et al. Evaluation of Eligibility Criteria Used to Identify Patients for Medication Therapy Management Services: A Retrospective Cohort Study in a Medicare Advantage Part D Population. J Manag Care Spec Pharm 2016;22:22-30. [Crossref] [PubMed]
- Abdela OA, Bhagavathula AS, Getachew H, et al. Risk factors for developing drug-related problems in patients with cardiovascular diseases attending Gondar University Hospital, Ethiopia. J Pharm Bioallied Sci 2016;8:289-95. [Crossref] [PubMed]
- Simonson W, Feinberg JL. Medication-related problems in the elderly: defining the issues and identifying solutions. Drugs Aging 2005;22:559-69. [Crossref] [PubMed]
- Kostis JB, Giakoumis M, Zinonos S, et al. Meta-Analysis of Usefulness of Treatment of Hypercholesterolemia With Statins for Primary Prevention in Patients Older Than 75 Years. Am J Cardiol 2020;125:1154-7. [Crossref] [PubMed]
- Deckx L, Kreijkamp-Kaspers S, McGuire T, et al. Chewing the fat over statins: Consumer concerns about lipid-lowering medication. Aust Fam Physician 2017;46:594-601. [PubMed]
- Wouters H, Van Dijk L, Geers HC, et al. Understanding Statin Non-Adherence: Knowing Which Perceptions and Experiences Matter to Different Patients. PLoS One 2016;11:e0146272. [Crossref] [PubMed]
- Lois-Martínez F, Fernandez-Alvarez O, Pérez-Vázquez C. El paciente polimedicado. Galicia Clin 2012;73:S37-41. [Crossref]
- Almodóvar AS, Nahata MC. Associations Between Chronic Disease, Polypharmacy, and Medication-Related Problems Among Medicare Beneficiaries. J Manag Care Spec Pharm 2019;25:573-7. [Crossref] [PubMed]
- Ferrer-Estrela F, Peris-Molina MT, Ubeda-Pascual A, et al. Algoritmo de actuación en la farmacia comunitaria para optimizar la utilización de estatinas. Pharmaceutical Care Españ 2015;17:272-86.
- Muñoz-Velandia OM, García-Peña ÁA (coords). Guía de práctica clínica para la prevención, detección temprana, diagnóstico, tratamiento y seguimiento de las dislipidemias en la población mayor de 18 años. Bogotá: Ministerio de Salud y Protección Social 2014.
- Gorodnycha O, Zimenkovsky A, Kostyana K. Drug-related problems associated with use of statins in Ukraine: a hospital-based study. PHARMACI 2016;63:29-34.
- Pallarés-Carratalá V, Pascual-Fuster V, Godoy-Rocatí D. Dyslipidaemia and vascular risk. A new evidence based review. Semergen 2015;41:435-45. [Crossref]
- Márquez-Contreras E, Gil-Guillén VF, De La Figuera-Von Wichmann M, et al. Non-compliance and inertia in hypertensive Spaniards at high cardiovascular risk: CUMPLE study. Curr Med Res Opin 2014;30:11-7. [Crossref] [PubMed]
- López-Simarro F, Brotons C, Moral I, et al. Inertia and treatment compliance in patients with type 2 diabetes in primary care. Med Clin (Barc) 2012;138:377-84. [PubMed]
- José Gagliardino J, Arechavaleta R, Goldberg Eliaschewitz F, et al. Dyslipidemia: The untreated metabolic dysfunction in people with type 2 diabetes in Latin America. ARETAEUS study outcomes. J Clin Transl Endocrinol 2019;15:76-80. [Crossref] [PubMed]
- Morales C, Plana N, Arnau A, et al. Causes of failure to achieve the low density lipoprotein cholesterol therapeutic target in patients with high and very high vascular risk controlled in Lipid and Vascular Risk Units. EROMOT study. Clin Investig Arterioscler 2018;30:1-9. [Crossref] [PubMed]
- Shawahna R, Odeh M, Jawabreh M. Factors Promoting Clinical Inertia in Caring for Patients with Dyslipidemia: A Consensual Study Among Clinicians who Provide Healthcare to Patients with Dyslipidemia. J Natl Med Assoc 2019;111:18-27. [Crossref] [PubMed]
- Lázaro P, Murga N, Aguilar D, et al. Therapeutic inertia in the outpatient management of dyslipidemia in patients with ischemic heart disease. The inertia study. Rev Esp Cardiol 2010;63:1428-37. [Crossref] [PubMed]
Cite this article as: Parody-Rúa E, Meneses-Torres A, Tyrovolas S. Problems related with the use the statins in primary health care, Cali-Colombia. J Public Health Emerg 2021;5:2.


