
Barriers and enablers to country adoption of National Surgical, Obstetric, and Anesthesia Plans
Introduction
This paper examines the adoption and diffusion of National Surgical Obstetric and Anaesthesia Plans (NSOAPs), a policy instrument, to improve surgical healthcare in low- and middle-income countries (LMIC). NSOAPs should be understood, simply, as flexible strategic planning processes that provide governments with an adaptable approach to guide health policies aimed at improving surgical healthcare within established institutional processes, political norms, population health needs, and economic constraints. From a strategic standpoint, the NSOAP could be better utilized to enhance the affirmation, visibility, integration, and alignment of surgical system objectives with the broader goals of the Ministry of Health (MoH) (e.g., reduce maternal mortality) and government at-large (e.g., poverty alleviation).
The NSOAP is a means (policy instrument) to an end (achieve surgical system objectives). Applying systems thinking (1) to the NSOAP process could enable policymakers and other stakeholders to more consistently and sustainably achieve this end; an end which has the potential to make considerable progress on the Sustainable Development Goals (SDGs) (2).
We organize this paper in two parts. Part one explores the relative progress of NSOAPs in terms of its adoption and diffusion in national health systems, using Atun’s systems framework of analyzing the integration of targeted interventions into health systems (3). In particular, we analyze the specificity of the health system as a distinct and critical mediating variable that influences—and ultimately determines—the adoption and diffusion of NSOAPs for surgical system reform, and thus requires for more serious consideration from an NSOAP design and implementation standpoint. Part two examines the unexplored opportunities for NSOAPs by applying systems thinking to enhance NSOAP adoption and diffusion, given recent adoption trends for NSOAPs, global health systems and broader political economy.
NSOAPs
“Surgical care is an indivisible, indispensable part of healthcare”, reported the Lancet Commission on Global Surgery (4). A key message of the Lancet Commission on Global Surgery report in 2015 was that surgical healthcare is a core component of national health systems; this argument contrasted starkly with the dominant perception (5,6) of surgical healthcare in global health discourse: it contested the notion that surgical healthcare was a marginal function of health systems as it was costly and rarely needed, especially by poor populations, which needed more “basic” healthcare services first (7).
A functional health system—that needs adequate financing, appropriate governance and organization, and a suitable level of human resources, infrastructure and data systems—is needed to deliver safe and affordable surgical healthcare services (4,8). Efforts aimed at improving surgical healthcare need to adopt a “systems” perspective. The Lancet Commission on Global Surgery recommended a generic approach for developing a national strategic plan (now commonly abbreviated as an NSOAP) to help “acknowledge the unknown” and guide the formation of a more “context-appropriate and comprehensive plan with time-bound targets” (7). The flexible NSOAP template provided general direction and an initial first step to mobilize interested stakeholders and establish surgical system priorities for countries seeking to improve surgical healthcare, using a systems approach.
Though the approach proposed by the Lancet Commission on Global Surgery was flexible and open for innovation, NSOAPs in practice have adhered to the template (9-12), followed a standard process and produced a similar set of normative conclusions (13). The final plans are technical documents; they present a series of costed health system changes (organized within the Lancet Commission on Global Surgery domains) to attain specific surgical system objectives and priorities reached through the NSOAP process (14). Once the plan is complete, the MoH is responsible for deciding how best to implement the proposed reforms across existing health programs. This appears to be a major challenge (13). The MoH must decide how best to finance, design, implement and evaluate an NSOAP in relation to several other competing priorities with varying levels of political risk, economic constraint, and citizen expectations.
Adoption of NSOAPs
By adoption, we refer to government entities prioritizing NSOAPs as a strategic process to improve surgical healthcare within a national or sub-national area. Though prioritisation is difficult to measure (15), it reflects the extent of political support for surgical healthcare and the likelihood of allocating long-term funding towards NSOAP implementation, within a government or regional entity (Box 1). Often, global and regional organizations, for example the World Health Organization (WHO) and Southern African Development Community (SADC) a regional economic zone of the African Union, can influence government priority by adopting resolutions and decisions related to surgical healthcare (16,17).
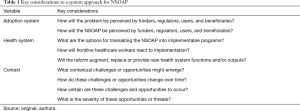
Full table
The MoH may demonstrate its institutional commitment by providing a specific department with the relevant authority to lead an NSOAP process, the development of an implementation plan following NSOAP formulation, and by incorporating aspects of an NSOAP into the National Health Strategic Plan to ensure that NSOAP activities are budgeted and implemented as part of the larger work of government.
At the time of writing, seven countries have developed NSOAPs, 12 were in process, and 32 nations had expressed varying forms of interest (18). To our knowledge, no country has developed sustainable health system financing mechanisms to fund an NSOAP. At regional level, two inter-governmental bodies have prioritized NSOAPs. In 2018 SADC, passed a resolution to improve surgical healthcare as a component of Universal Health Coverage (UHC) (17). Each of the 16 SADC Member States report on NSOAP progress annually at the annual SADC Health Minister and Senior Officials meeting. Member States of the World Health Organization Western Pacific Regional Committee endorsed the Regional Action Framework for Achieving Safe and Affordable Surgery in the Western Pacific Region [2021−2030] at the 71st Regional Committee Meeting in October 2020 (19,20).
Diffusion of NSOAPs
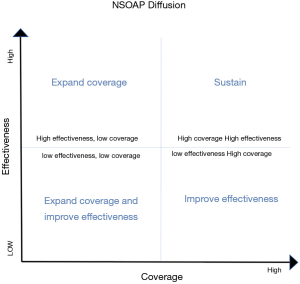
Diffusion relates to the extent to which the strategic recommendations of NSOAPs have improved surgical system performance (effectiveness) and scaled-up to reach large populations for impact (coverage) (Box 1). These dimensions could be used to develop a matrix that depicts the extent of NSOAP diffusion over time (Figure 1). Though such an assessment may be premature currently (NSOAPs are relatively new with meagre funding allocated for their implementation, with funding constrained due to COVID-19) this approach could be used in future assessments (21,22). At this early stage, NSOAP diffusion has not occurred to a significant extent. To enable diffusion and real-world impact, NSOAPs need to be translated into implementable programs that are sustainably funded and implemented in a coordinated manner across other existing MoH programs.

Full table
A “systems” approach to NSOAP adoption and diffusion
The health system is the key intervening variable, influencing the adoption and diffusion of health care reforms (23). What are health systems and how do health system attributes and characteristics influence NSOAP diffusion?
Health systems exhibit the properties of a complex system (24,25). The introduction of change—a new process (integrated care), subject (nurses, doctors), object (devices, medicines, diagnostics) or structure (organizational function and institutional arrangement)—produces different results over time and varying effects on different parts of the health system (3,25,26). Health systems are characterized by (I) interdependent and interconnected linkages and networks, and; (II) system attributes and properties as a whole, which are larger and more complex than the sum of its constituent parts (23). These characteristics lead to both non-linear and bidirectional interactions between cause and effect. A health system, like any complex adaptive system, strives to maintain an equilibrium: change is often resisted, altering the balance of forces to produce a net “system response”, with both desirable and unintended effects—and bounded predictability (23).
These health system attributes influence both the rate and extent of integration of new health policies, processes, devices, organizational practices, and ideas into programs that ultimately deliver care to patients (3). A health system is embedded within a broader context (26,27) creating an environment of “dynamic complexity”, an interplay which creates both opportunities and threats to a health system (23,25,28,29). These contextual factors produce the net effect of either enabling the change or generating resistance to achieve an equilibrium. Indeed, the same contextual factor may be enabling over the short-term but threatening over the long-term.
This dynamic interplay inherent in health systems, which comprise people and institutions within a continually evolving context, influences the extent of resistance to NSOAP adoption (failure to adopt) and unanticipated results (failure to diffuse). The “system response” may resist the NSOAP (e.g., an inability to fund an NSOAP) or produce unexpected results, varying effects on the health system (e.g., increased uptake of unsafe surgical healthcare services, may lead to worse health outcomes), and time-dependent consequences (short-term expanded workforce leading to physician emigration over the longer-term in the absence of adequate incentives to promote retention).
Applying systems thinking to enable NSOAP adoption and diffusion
Linear, rigid, and overly technical approaches to NSOAPs, which fail to recognize the interrelated elements of health systems and contextual factors that comprise the real-world, may lead to failure to adopt and diffuse (23,27,28,30). We provide a framework to apply a health systems approach to NSOAPs for enhanced adoption and diffusion. Such an approach could allow for enhanced framing, design, strategy and agility in the implementation process. The framework consists of three components concerning the NSOAP (Figure 2):
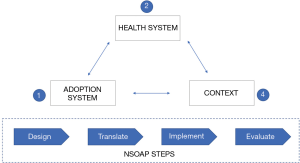
- Adoption system;
- Health system;
- Context.
The NSOAP process consists of four steps: design, translate, implement, evaluate (Figure 2). The adoption system consists of the key actors or markets that pay, regulate, use, or benefit from, the NSOAP. The health system refers to the set of institutions whose primary intent is to improve the overall level of health in a society. It consists of institutions and individuals that mobilize health system resources and convert them into both public and personal health services that improve population health, reduce financial catastrophe, and improve user satisfaction (29). Established care pathways exist at different (and between) levels of the health system to enable health systems to provide both personal and population health services to attain these goals. The context consists of the political, economic, ecological, technological and socio-cultural milieu (29), which present both challenges and opportunities to either enhance or resist the NSOAP. Table 1 outlines the key considerations within each of three components to be iteratively analyzed throughout the NSOAP process. The rate and extent of NSOAP adoption and diffusion is determined by its interaction with these three components—adoption system, health system and broader context.
Adoption system
NSOAPs may need to be oriented towards the dominant actors within the adoption system. Reorientation may occur in terms of the problem framing or positioning of the proposed solutions to enhance the perceptions of the NSOAP within the adoption system. These actors include individuals and institutions in the health system and broader context who are responsible for funding, regulating, using or the beneficiaries themselves of the resulting programs. Funders could include actors from the public, private or voluntary sectors. If a government seeks to expand surgical healthcare through UHC, the NSOAP could focus on developing an essential surgical package to be included in the standard benefits package (31).
The NSOAP should be titled and framed according to how it will be positioned and in relation to what it seeks to achieve. Regulatory entities provide the rules (provider accreditation, education and training, payment, medico-legal processes), which will influence the introduction of the program into the health system. For instance, allowing citizens in a UHC system to purchase surgical healthcare services from private providers will require negotiating fair terms of service provision and payment of providers (32). The surgeons, anesthesiologists, nurses and allied health workers (the users) will resist changes if the proposed reforms jolt the established institutional logic and conventional paradigm of work (33). Finally, patients themselves should be the focus of patient-centered care, grounded in a sturdy primary health care foundation that includes demand-side interventions and the social determinants of health. Thinking through their care needs, could help to develop innovative delivery mechanisms that produce targeted approaches to surgical healthcare, improving health system efficiency (34). In dynamic contexts, the NSOAP will need to iteratively reorient, and at times, reconfigure its positioning to manage a strong base of support for the NSOAP through the various steps. For instance, while funders may be of principal significance throughout the process, the users (practitioners) are invaluable when translating the NSOAP into implementable activities. A strong investment case should support the framing of the problem (scale, scope and health and economic consequences of inaction) and proposed solution that is well-aligned to the problem.
Health system
When translating the NSOAP into health programs, health system characteristics need to be considered to increase receptiveness to the proposed changes. When introducing new structures, functions and service delivery mechanisms to the health system, NSOAP planners and implementers ought to consider how it will influence existing structures, functions and care pathways and how it will be perceived by key individuals and institutions (33). Inadequate consideration will disrupt the equilibrium and produce negative balancing, or corrective effects, which will resist the NSOAP. Practically, this implies thinking through how new programs will change existing structures, functions and care pathways, predicting responses, and taking remedial actions to minimize resistance. For instance, if the reform increases access to surgical healthcare services in the context of high levels of physician burnout and frustration, corresponding actions need to be taken to raise physician satisfaction, through either monetary or non-monetary incentives and factoring in the pull and push factors of physician migration. Implementation and scale-up should focus on anticipating issues rather than dealing with consequences. Finally, it should be clear and continually measured, how the proposed program addresses the specific problem it was designed to solve.
Context
The context influences health system dynamics and includes political, economic, social, technological, ecological, epidemiological, demographics and legal factors (29). An economic recession will reduce fiscal space, making increasing expenditure on a comprehensive national surgical reform effort challenging (35). Conversely, a sustained favorable economic outlook may create the needed fiscal space to increase expenditure on expanding UHC (36) through surgical healthcare. Technological advances may radically alter the delivery of diagnostics needed for surgical healthcare (37), but may also create complex workflow arrangements that hamper physician creativity (38). Contextual factors could be analyzed and mapped throughout the NSOAP process to leverage opportunities and take mitigation actions to curb the effects of emergent threats.
NSOAPs 2.0: applying systems-thinking across the NSOAP process
Practitioners involved in the NSOAP steps (design, translate, implement and evaluate) could harness systems thinking to enhance the receptivity, adoption and diffusion of NSOAPs to improve health system performance. At this juncture in the adoption and diffusion of NSOAPs, three strategic considerations could be explored.
Data and digital technology
The NSOAP design process consists of two fundamental steps: (I) quantifying gaps in surgical healthcare. This is achieved through a situation analysis; (II) setting priorities to fill the gaps in surgical healthcare. This step is achieved through a priority-setting process with varying stakeholder representation and form of priority-setting practices. The appropriate application of digital technology to existing data could help to simplify both steps and make the process nimbler and more effective. For many LMICs, there are existing data sets at a global, regional, national, and sub-national level, which could be utilized better to quantify gaps in the surgical workforce, infrastructure, funding, service delivery, and governance (39). Expensive, time-consuming and human resource-heavy approaches to quantify the surgical gap are often not feasible or efficient in most LMICs, especially when considering the health system as a complex system (40). Simple and accurate visual data platforms could be developed from existing data and cloud computing used to standardize the collection, pooling, and analysis of information needed to assess the performance of surgical systems.
Priority-setting could be streamlined by aligning with existing health system planning processes and enabling decisions based on simulations that take into account the complex nature of scenario projection in health systems (40). Quickly identifying the major problem areas within political, economic and technical constraints is vital to enabling efficient priority-setting processes. Since many governments have existing policies in which strengthening surgical healthcare could be integrated, priorities to improve surgical healthcare could be embedded within these strategies. Low-cost and open source artificial intelligence and machine learning platforms could be developed, using non-biased, transparent, modifiable, and explainable algorithms (41), to assist health system planners in making resource-allocation decisions based on definable parameters (39).
Financing
Fiscal space to fund NSOAPs is constrained in most LMICs (22). COVID-19 has exacerbated the problem, both due to its direct economic effects, but also due to changing political attitudes in relation to surgical healthcare and immediate healthcare needs. Nevertheless, since there will always be finite resources available to fund an NSOAP, it is vital to quantify potential fiscal space available, determine the sources, and then develop an overall strategy to mobilize such funding. These objectives can be achieved by developing a financing strategy for surgical health care before embarking upon the NSOAP and modified throughout the NSOAP process (42). Understanding the funding constraints, will help to keep the NSOAP recommendations within the fiscal envelope, which influences health system financing. There are also opportunities to improve spending efficiency and public finance management in the health sector—a key driver of imprudent expenditure in emerging economies (35,36). Evaluating how surgical system resources relate to surgical outcomes, will reveal options for most cost-efficient intervention for investment. For example, in a country in which supply chain mismanagement contributes to health sector spending inefficiency, the NSOAP could introduce blockchain technology to improve the transparency and accountability in the procurement, delivery and use of surgical supplies and goods. Innovative financing has been explored, but not yet designed, introduced and scaled-up to channel substantial funding to surgical healthcare at the national level.
Governance and management
NSOAP effectiveness is only as good as the policies designed to improve surgical healthcare are implemented. Governance is a significant, though not well examined, mediating variable which can influence NSOAP implementation through four channels: (I) degree to which the NSOAP activities (and what specific NSOAP activities) become embedded within national health plans; (II) procurement of NSOAP-related infrastructure; (III) surgical system resource allocation decisions; (IV) capability of health managers to implement at facility level. A much more comprehensive assessment of how each of these factors could be optimized should be factored into costing and included in governance recommendations of the NSOAP.
At a management level, it is prudent to consider who will be involved in each NSOAP step. In several SADC countries, NSOAP teams are comprised of physicians that support the NSOAP process, beyond their regular working hours. These NSOAP teams should be supported and funded to promote an enabling working environment and employed in a manner that promotes their sustained contribution, with appropriate incentives and within an established institution (for instance the MoH). Teams could employ different management approach’s, for instance agile methods, which have improved team efficiency, innovation, productivity and team satisfaction in various business sectors from software development and manufacturing to healthcare (43,44). Agile team management approaches could help prioritize activities, generate and test innovative ideas, simplify processes and iteratively modify the NSOAP throughout each step. Such an approach, could enable enhanced responsiveness to changes in the health system (e.g., new rules affecting public and private provision of healthcare services) and broader context (e.g., new political leadership pursuing different policies).
Conclusions
NSOAP adoption and diffusion as a policy instrument has been constrained by two factors: (I) suboptimal funding and (II) inadequate translation of the NSOAP into implementable activities. Systems thinking—adapting and optimizing the NSOAP steps to health system characteristics, adoption system, and the broader context—may enhance the adoption and diffusion of NSOAPs. There exist opportunities to leverage technology, financing, and governance to translate NSOAPs into context-sensitive healthcare programs that people value and which contribute towards improving surgical healthcare over the long-term.
Acknowledgments
We are deeply grateful to Kee B. Park, Zachary Fowler and Rennie Qin from the Program in Global Surgery and Social Change at Harvard Medical School for fact-checking NSOAP progress in the Western Pacific Region.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Dominique Vervoort) for the series “Global Surgery” published in Journal of Public Health and Emergency. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form, available at: http://dx.doi.org/10.21037/jphe-2021-02. The series “Global Surgery” was commissioned by the editorial office without any funding or sponsorship. All authors have no other conflicts of interest to declare.
Financial Disclosure: None. The Program in Global Surgery and Social Change receives funding from the GE Foundation as part of the SS2020 program, unrelated to this manuscript.
Ethical Statement: All authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Checkland P. Systems thinking, systems practice. Chichester; New York: Wiley, 1981:xiv+330.
- Roa L, Jumbam DT, Makasa E, et al. Global surgery and the sustainable development goals. Br J Surg 2019;106:e44-52. [Crossref] [PubMed]
- Atun R, De Jongh T, Secci F, et al. Integration of targeted health interventions into health systems: A conceptual framework for analysis. Health Policy and Planning 2010;25:104-11. [Crossref] [PubMed]
- Meara JG, Leather AJM, Hagander L, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet 2015;386:569-624. [Crossref] [PubMed]
- Farmer PE, Kim JY. Surgery and Global Health: A View from Beyond the OR. World J Surg 2008;32:533-6. [Crossref] [PubMed]
- Petersen PE. World Health Organization. Organisation Mondiale de la Sante. Commun Dent Oral Epidemiol 2003;31:471. [Crossref]
- Mukherjee JS, Mugunga JC, Shah A, et al. A practical approach to universal health coverage. Lancet Global Health 2019;7:e410-1. [Crossref] [PubMed]
- Citron I, Sonderman K, Subi L, et al. Making a case for national surgery, obstetric, and anesthesia plans. Canadian Journal of Anesthesia/Journal canadien d’anesthésie 2019;66:263-71.
- Tanzania National Surgical, Obstetric and Anaesthetic Plan: 2018-2025 [Internet]. Ministry of Health, Community Development, Gender, Elderly and Children, Government of Tanzania; 2018. Available online: https://docs.wixstatic.com/ugd/d9a674_4daa353b73064f70ab6a53a96bb84ace.pdf
- Zambian National Surgical, Obstetric, And Anaesthesia Strategic Plan (NSOASP) Year 2017-2021 [Internet]. Republic of Zambia Ministry of Health.; Available online: https://docs.wixstatic.com/ugd/d9a674_70f6813fe4e74c4d99eb028336a38745.pdf
- Nigeria National, Obstetric and Anaesthesia Plan: 2019-2023 [Internet]. Federal Ministry of Health, Government of Nigeria; Available online: https://docs.wixstatic.com/ugd/d9a674_1f7aa8161c954e2dbf23751213bc6f52.pdf
- Rwanda National, Obstetric and Anaesthesia Plan: 2018-2024 [Internet]. Ministry of Health, Government of Rwanda; Available online: https://docs.wixstatic.com/ugd/d9a674_c5c36059456a416480fd58fd553ef302.pdf
- Peters AW, Roa L, Rwamasirabo E, et al. National Surgical, Obstetric, and Anesthesia Plans Supporting the Vision of Universal Health Coverage. Glob Health Sci Pract 2020;8:1.3-9.
- Implementing World Health Assembly Resolution 68.15: National surgical, obstetric, and anesthesia strategic plan development—the Zambian experience [Internet]. The Bulletin 2017 [cited 2019 Feb 20]. Available online: http://bulletin.facs.org/2017/06/implementing-world-health-assembly-resolution-68-15/
- Shawar YR, Shiffman J, Spiegel DA. Generation of political priority for global surgery: a qualitative policy analysis. Lancet Global Health 2015;3:e487-95. [Crossref] [PubMed]
- 68th World Health Assembly. WHA 68.15 Strengthening emergency and essential surgical care and anaesthesia as a component of universal health coverage. Provisional agenda item 51 2015;(May 26):16-8.
- SADC secretariat. Media Statement - Joint Meeting of SADC Ministers of Health 2018 [Internet] 2018 [cited 2020 Jul 10]. Available online: https://www.sadc.int/files/3315/4169/8409/Media_Statement_-_Joint_Meeting_of_SADC_Ministers_of_Health_and_those_responsible_for_HIV_and_AIDS_.pdf
- Roa L, Peters AW, Meara JG. National Surgical, Obstetric and Anesthesia Planning for High-Level Global, Regional, and Country Authorities and Funders: Proceedings. Dubai: Harvard Medical School Center for Global Health Delivery-Dubai; 2019.
- World Health Organization. Resolution: Safe And Affordable Surgery [Internet]. WPR/RC71.R2 Oct 9, 2020. Available online: https://www.who.int/docs/default-source/wpro---documents/regional-committee/session-71/rc71-r2-safe-and-affordable-surgery.pdf
- Virtual Consultations To Develop The Regional Action Framework For Achieving Safe And Affordable Surgery In The Western Pacific Region (2021-2030). Manila, Philippines: World Health Organization Regional Office for the Western Pacific; 2020 Mar p. 17. Report No.: RS/2020/GE/09(PHL).
- Jumbam DT, Reddy CL, Roa L, et al. How much does it cost to scale up surgical systems in low-income and middle-income countries? BMJ Glob Health 2019;4:e001779 [Crossref] [PubMed]
- Reddy CL, Peters AW, Jumbam DT, et al. Innovative financing to fund surgical systems and expand surgical care in low-income and middle-income countries. BMJ Glob Health 2020;5:e002375 [Crossref] [PubMed]
- Atun R. Health systems, systems thinking and innovation. Health Policy and Planning 2012;27:iv4-8. [Crossref] [PubMed]
- Forrester JW. Industrial dynamics. Cambridge, Mass.: MITPress; 1961. 464 p.
- Atun RA, Menabde N, Saluvere K, et al. Introducing a complex health innovation—Primary health care reforms in Estonia (multimethods evaluation). Health Policy 2006;79:79-91. [Crossref] [PubMed]
- Atun RA, Kyratsis I, Jelic G, et al. Diffusion of complex health innovations--implementation of primary health care reforms in Bosnia and Herzegovina. Health Policy Planning 2007;22:28-39. [Crossref] [PubMed]
- Massuda A, Hone T, Antonio F, et al. The Brazilian health system at crossroads: progress, crisis and resilience 2018;1-8.
- Doniec K, Dall’Alba R, King L. Austerity threatens universal health coverage in Brazil. Lancet 2016;388:867-8. [Crossref] [PubMed]
- Atun R, Aydin S, Chakraborty S, et al. Universal health coverage in Turkey: Enhancement of equity. Lancet 2013;382:65-99. [Crossref] [PubMed]
- . The hope for a new dawn for South Africa. Lancet 2018;391:714. [Crossref] [PubMed]
- Reddy CL, Vervoort D, Meara JG, et al. Surgery and universal health coverage: Designing an essential package for surgical care expansion and scale-up. J Glob Health 2020;10:020341 [Crossref] [PubMed]
- OECD, World Health Organization, Barber SL, Lorenzoni L, Ong P. Price Setting and Price Regulation in Health Care [Internet]. OECD; 2019 [cited 2020 Dec 10]. Available online: https://www.oecd-ilibrary.org/social-issues-migration-health/price-setting-and-price-regulation-in-health-care_ed3c16ff-en
- Kyratsis Y, Atun R, Phillips N, et al. Health Systems in Transition: Professional Identity Work in the Context of Shifting Institutional Logics. Academy Management J 2017;60:610-41. [Crossref]
- Geldsetzer P, Manne-Goehler J, Theilmann M, et al. Geographic and sociodemographic variation of cardiovascular disease risk in India: A cross-sectional study of 797,540 adults. PLoS Med 2018;15:e1002581 [Crossref] [PubMed]
- Barroy H, Sparkes S, Dale E, et al. Can Low- and Middle-Income Countries Increase Domestic Fiscal Space for Health: A Mixed-Methods Approach to Assess Possible Sources of Expansion. Health Systems Reform 2018;4:214-26. [Crossref] [PubMed]
- Tandon A, Cashin C. Assessing public expenditure on health from a fiscal space perspective [Internet]. Washington, DC: World Bank; 2010. (Health, Nutrition and Population (HNP) discussion paper). Report No.: 56053. Available online: http://documents.worldbank.org/curated/en/333671468330890417/Assessing-public-expenditure-on-health-from-a-fiscal-space-perspective
- Oktay O, Nanavati J, Schwaighofer A, et al. Evaluation of Deep Learning to Augment Image-Guided Radiotherapy for Head and Neck and Prostate Cancers. JAMA Netw Open 2020;3:e2027426 [Crossref] [PubMed]
- Collier R. Electronic health records contributing to physician burnout. CMAJ 2017;189:E1405-6. [Crossref] [PubMed]
- Reddy CL, Mitra S, Meara JG, et al. Artificial Intelligence and its role in surgical care in low-income and middle-income countries. Lancet Digital Health 2019;1:e384-6. [Crossref] [PubMed]
- Forrester JW. System dynamics, systems thinking, and soft OR. System Dynamics Rev 1994;10:245-56. [Crossref]
- Panch T, Szolovits P, Atun R. Artificial intelligence, machine learning and health systems. J Glob Health 2018;8:020303 [Crossref] [PubMed]
- Reddy CL, Jumbam DT, Meara JG, et al. A Financing Strategy to Expand Surgical Healthcare. BMJ Glob Health 2020;5:e002375 [Crossref] [PubMed]
- Embracing Agile. Harvard Business Review [Internet] 2016 May 1 [cited 2021 Feb 7]; Available online: https://hbr.org/2016/05/embracing-agile
- How Agile Is Powering Healthcare Innovation [Internet]. Bain 2019 [cited 2021 Feb 7]. Available online: https://www.bain.com/insights/how-agile-is-powering-healthcare-innovation/
Cite this article as: Reddy CL, Miranda E, Atun R. Barriers and enablers to country adoption of National Surgical, Obstetric, and Anesthesia Plans. J Public Health Emerg 2021;5:18.


