
A family cluster of pediatric cases of severe fever with thrombocytopenia syndrome following short-time exposure to a city park in China: case reports
Introduction
Severe fever with thrombocytopenia syndrome (SFTS), a new tick-borne zoonosis caused by severe fever with thrombocytopenia syndrome virus (SFTSV), is characterized by fever, thrombocytopenia, leukopenia and gastrointestinal symptoms (1,2). SFTSV is primarily transmitted to humans by exposure to or bitten by infected ticks (3-5), while the secondary cases can also be infected by person-to-person transmission with possible inhalation of virus-containing aerosol (6), or direct contact with blood or bloody secretions carrying SFTSV (7,8). SFTS usually occurs as sporadic cases, and clustered cases occur less frequently (9). Meanwhile, elderly people in rural areas with hills and mountains have the greatest risk of acquiring SFTS (2,10-12). Here, we described a family cluster of two pediatric cases of SFTS following short-time exposure to a city park in Jiangsu Province, and analyzed the clinical and epidemiological characteristics of these two cases.
We present the following article in accordance with the CARE reporting checklist (available at https://jphe.amegroups.com/article/view/10.21037/jphe-21-41/rc).
Case presentation
Case detection and investigation
Two children from the same family in Lishui District, Jiangsu Province, were diagnosed with suspected SFTS cases by a doctor of Nanjing Children’s Hospital, since they had fever, leukopenia and thrombocytopenia. Then their serum specimens were collected and sent to the laboratory in Jiangsu Provincial Center for Disease Control and Prevention (CDC). Finally, SFTSV-specific RNA was detected from the serum specimens of them. After anti-virus and anti-infective therapy (use ribavirin and moxalactam respectively) and other supportive treatment, they all recovered well without sequelae being observed.
After receiving the case report, Lishui District CDC, Nanjing Municipal CDC, and Jiangsu Provincial CDC jointly conducted an epidemiological investigation into this family cluster of laboratory-confirmed SFTS cases, including inquiring about the cases’ clinical and laboratory characteristics, living surroundings, history of tick bites and animal contacts, and the routes of possible exposure to risk factors. Their father and medical staff were also interviewed.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Oral informed consent was obtained from the patients’ parents.
Case description
Case 1
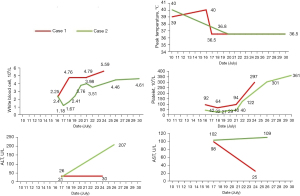
Case 1 was a 5-year-old boy who experienced sudden onset fever with the highest temperature of 39 ℃ at night on 10 July 2018. The boy was admitted to People’s Hospital of Lishui District on 13 July 2018, where he received treatment for 3 days. On 16 July, the boy was transferred to Nanjing Children’s Hospital because of persistent and high fever with the highest temperature of 40 ℃ and cough. He had leukopenia (white blood cell count, 2.25×109/L) and thrombocytopenia (platelet count, 92×109/L), elevated liver-associated enzyme levels (glutamic oxaloacetic transaminase, 98 U/L) and positive urine protein. The boy was diagnosed with bronchitis according to his clinical symptoms and chest X-ray examination, no gastrointestinal and hemorrhagic symptoms were observed. He was diagnosed with SFTSV infection on 17 July 2018, then he was treated with moxalactam and other symptomatic and supportive treatment. His temperature began to drop to the normal range (around 36.5 ℃) on the same day. On 18 July, the boy’s white blood cell count raised to 4.76×109/L. On 24 July, his platelet count raised to 297×109/L, his glutamic oxaloacetic transaminase had declined to 25 U/L and urine protein turned negative. Finally, the boy was discharged on 25 July.
Case 2
Case 2 was a 15-year and 6-month-old girl who had experienced a sudden onset fever with the highest temperature of 40 ℃ on 10 July 2018. She was admitted to People’s Hospital of Lishui District on 13 July. With persistent and high fever after 3 days of treatment, she was transferred to Nanjing Children’s Hospital on 16 July. She had leukopenia (white blood cell count, 2.40×109/L) and thrombocytopenia (platelet count, 42×109/L), then she was diagnosed with SFTSV infection on 17 July and she was treated via moxalactam, ribavirin and other symptomatic and supportive treatment. The girl’s illness was more serious than that of her brother, her white blood cell count and blood platelet count decreased rapidly to 1.18×109/L on 17 July and 27×109/L on 18 July, respectively. Her urine protein presented positive on 22 July. She did not exhibit any symptoms of dyspnea, consciousness disorder, dizziness, or hemorrhage. The girl's body temperature turned to normal (around 36.5 ℃) on 20 July, her white blood cell and platelet finally returned to normal range with the white blood cell count of 4.46×109/L on 24 July and platelet count of 122×109/L on 22 July. Laboratory testing indicated that her urine protein presented negative on 26 July, but her liver enzyme was still above normal range (glutamic-pyruvic transaminase, 207 U/L; glutamic oxaloacetic transaminase, 109 U/L. Anti-virus and anti-infective therapy (use ribavirin and moxalactam respectively) were discontinued since 27 July. Then the doctor approved her parents’ asking for leaving the hospital. Followed-up observation showed the girl got well recovered after a period of time.
Dynamic profiles of clinical indicators [peak temperature, white blood cell, platelet, alanine aminotransferase (ALT), aspartate aminotransferase (AST)] of two SFTS pediatric cases are shown in the Tables 1,2 and Figure 1.
Table 1
| Clinical feature | 10 July | 16 July | 17 July | 18 July | 19 July | 20 July | 21 July | 22 July | 23 July | 24 July | 25 July (discharge) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Peak temperature (℃) | 39 | 40 | 36.5 | 36.5 | 36.5 | 36.5 | 36.5 | 36.5 | 36.5 | 36.5 | 36.5 |
| Malaise | N | Y | Y | Y | Y | N | N | N | N | N | N |
| Cough | N | Mild | Mild | Mild | Mild | Mild | Mild | N | N | N | N |
| Pharyngeal swelling | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | N |
| Antiadoncus | N | N | N | N | N | I° | I° | I° | N | N | N |
| Astriction | N | N | N | N | Y | Y | Y | N | N | N | N |
| Laboratory variables | |||||||||||
| White blood cells (×109/L) | – | 2.25 | – | 4.76 | – | – | 4.79 | – | – | 5.59 | – |
| Platelets (×109/L) | – | 92 | – | 64 | – | – | 94 | – | – | 297 | – |
| ALT (U/L) | – | – | 31 | – | – | – | – | – | – | 30 | – |
| AST (U/L) | – | – | 98 | – | – | – | – | – | – | 25 | – |
| Positive urine protein | + | + | − |
Y, yes; N, no; I°, the least severe grade of antiadoncus; ALT, alanine aminotransferase; AST, aspartate aminotransferase.
Table 2
| Clinical feature | 10 July | 16 July | 17 July | 18 July | 19 July | 20 July | 21 July | 22 July | 24 July | 26 July | 27 July | 29 July | 30 July (discharge) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Peak temperature (℃) | 40 | – | – | – | 36.8 | 36.5 | 36.5 | 36.5 | 36.5 | 36.5 | 36.5 | 36.5 | 36.5 |
| Malaise | N | N | N | N | Y | Mild | N | N | N | N | N | N | N |
| Pharyngeal swelling | N | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N |
| Antiadoncus | N | N | I° | I° | I° | I° | I° | I° | N | N | N | N | I° |
| Nausea and vomiting | N | Y | Y | Y | Y | Y | N | N | N | N | N | N | N |
| Anepithymia | N | Y | Y | Y | Y | Y | N | N | N | N | N | N | N |
| Astriction | N | N | N | Y | Y | N | N | N | Y | N | N | N | N |
| Laboratory variables | |||||||||||||
| White blood cells (×109/L) | – | 2.40 | 1.18 | 1.67 | 2.41 | 3.76 | 3.98 | 3.51 | – | 4.46 | – | – | 4.61 |
| Platelets (×109/L) | – | 42 | 32 | 27 | 29 | 40 | 40 | 122 | – | 301 | – | – | 361 |
| ALT (U/L) | – | – | 26 | – | – | – | – | – | – | 207 | – | – | – |
| AST (U/L) | – | – | 102 | – | – | – | – | – | – | 109 | – | – | – |
| Positive urine protein | + | + | − |
Y, yes; N, no; I°, the least severe grade of antiadoncus; ALT, alanine aminotransferase; AST, aspartate aminotransferase.
Epidemiology
These two cases lived in the center of Baima town (with a population of 39,859 in 2017) in Lishui District of Nanjing City, Jiangsu Province. This district has a high incidence of SFTS, where 46 SFTS confirmed cases were reported from 2010 to 2018, accounting for 18.78% of the total cases in Jiangsu Province according to surveillance data from Jiangsu Provincial CDC.
These two cases lived in a high-rise building with a green belt in the residential area. According to their parents, they had used to take exercise and play on the green belt. However, no similar cases were reported in their residential area, and they had no contact with a similar patient before illness onset. Epidemiological investigation showed that these two children had played in a city park. They complained about no clear history of insect bites, and no skin itching or redness and other discomfort symptoms during the play.
We collected questing ticks by using tick drags (1×1 m2 white cotton flannel cloth) on the residential area’s green belt of these two cases and the city park lawn. Three questing ticks were caught on the city park lawn, but no ticks were caught on the residential area’s green belt. Although these ticks were identified as Haemaphysalis longicornis, the results were negative in SFTS-RNA detection in these ticks.
Viral RNA extraction and detection
Acute phase blood samples were collected from the suspected SFTS patients. Sera were separated from the blood samples by centrifugation at 3,500 rpm for 5 min. RNA was extracted from 140 μL serum samples using QIAamp Viral RNA Mini kit (Qiagen, Hilden, Germany) according to the manufacturer’s instructions. SFTSV RNA were detected with a real-time RT-PCR assay previously described using QuantiTect Probe RT-PCR Kit (Qiagen, Hilden, Germany) (13). The conditions for real-time RT-PCR reaction were as follows: 50 ℃ for 30 min, 95 ℃ for 10 min, 45 cycles of 95 ℃ for 15 s, 55 ℃ for 40 s. Data were analyzed using the software supplied by the manufacturer.
SFTSV genome sequencing and phylogenetic analysis
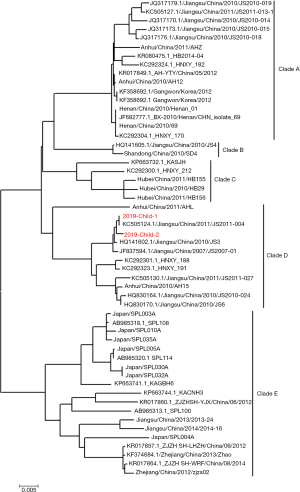
Complete sequencing of M segment of SFTSV strain was performed using primers as previously described (13). The RT-PCR products were sent to Sangon Biotech (Shanghai, China) for Sanger DNA sequencing. The termini of viral RNA segments were determined with the First Choice RLM-RACE Kit (Invitrogen, USA). Phylogenetic analysis was conducted based on the M segments of SFTSV. Sequences were aligned using Cliustal W. The phylogenetic trees were constructed using the Maximum Likelihood Method with the MEGA5.1 software based on M segments of SFTSV strains from different SFTS endemic areas. The reliability values indicated at the branch nodes were determined using 1,000 bootstrap replications. The red taxon names of the phylogenetic trees presented SFTSV strains isolated in this study.
Blast comparison showed that both of these two new strains (2019 child 1 and 2019 child 2) were close to SFTSV strains from Jiangsu province. The two M segments in this study shared high nucleotide similarity with strain Jiangsu/China/2011/JS2011-004 (99.2% and 99.1%), which was isolated from a local patient in Lishui in 2011. The boy’s M segment wasn’t exactly the same as his sister’s. Phylogenetic analysis showed that both of the two new strains belonged to Clade D genotype based on the maximum likelihood tree of M segments (Figure 2). These results suggested that these two cases were infected with SFTSV from the local area.
Discussion
This report described a family cluster of pediatric cases of SFTS. We speculate that two cases’ short-time exposure to the city park lawn was the main cause of this cluster. There are three reasons present as follows. Firstly, these two cases were exposed to the city park lawn at the same time and they got sick on the same day. The interval from exposure to illness onset was five days, which was consistent with the incubation period of SFTS (14). Secondly, the longhorned tick, namely Haemaphysalis longicornis, the most abundant human-biting tick species in most SFTS-endemic areas of China, is known as the major vector (8,9). We found Haemaphysalis longicornis ticks on the city park lawn, although the SFTS-RNA detection was negative in these ticks, maybe caused by small sample size. Last but not least, with no SFTS cases reported in the children’s residential area and no ticks have been collected from the green belt where they used to play, the two children were less likely to be infected by exposure to the green belt of their residential area.
According to their clinical symptoms mentioned above, children’s illnesses suffered from SFTS were relatively mild compared with adult SFTS cases. They did not exhibit dyspnea, consciousness disorder, dizziness, or gastrointestinal and hemorrhagic symptoms. In addition, the onset of thrombocytopenia was also delayed for pediatric cases than in adults (about 7 days after disease onset vs. 1 to 2 days, respectively), which was consistent with the previously report of pediatric cases of SFTS (15-17). Besides, two children in this cluster all have the symptoms of elevated liver-associated enzyme level and positive urine protein, which were similar to adults who infected with SFTSV, these could be caused by virus infection and long-term antiviral treatment after admission (18).
The result of the genetic sequencing was something representation based on these two cases’ common exposure history and pathogenesis. Phylogenetic analysis showed that both of the two new strains were belonged to Clade D genotype, although the boy’s M segment wasn’t exactly the same as his sister’s. These results suggested that both of these two cases were infected with SFTSV from the local area, while there was no human-to-human transmission of infection between them. High nucleotide similarity (99.2% and 99.1%) between the M segments of the two cases and a local patient in Lishui in 2011 suggested that these children were infected with SFTSV from the local area and this sequence of SFTS may have already exist in the hills or mountains areas of Lishui in 2011 and then it transported to the other areas such as city park visa human or animal migration later. The infection of this two SFTS pediatric cases suggests that the city park could become a new endemic area of SFTS, which was rarely mentioned by previous studies.
In our report, we revealed a family cluster of pediatric cases of SFTS in Lishui District of Nanjing City, Jiangsu Province. This cluster of SFTS was firstly revealed of pediatric cases with possible infection risk factor of exposure to the city park lawn which suggests that the city park could become a new endemic area of SFTS. Besides, we found the children’s illness suffered from SFTS were relatively mild compared with adult SFTS cases. We also carried out propaganda and disseminated knowledge about SFTS among nearby residents. Close attention and further study should be conducted to provide reference for the following prevention and treatment of SFTS.
Acknowledgments
We thank all the clinical and epidemiological personnel for investigating and reporting the information on SFTS cases. We appreciate the public health institution of county-level for their disease surveillance, investigation and correction of the epidemiological information.
Funding: This work was supported partly by Natural Science Foundation of China (No. 81601794 & No. 81703284), Jiangsu Provincial Key Medical Discipline of Epidemiology (No. ZDXKA2016008), Jiangsu Provincial Medical & Youth Talent (No. ZDRCA2016032 & QNRC2016545), Jiangsu Provincial Nature Science Foundation (No. BK20161584), “Six One Project” Top Talent Research Plan of Jiangsu High Level Health Talents (No. LGY2019073).
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://jphe.amegroups.com/article/view/10.21037/jphe-21-41/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jphe.amegroups.com/article/view/10.21037/jphe-21-41/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Oral informed consent was obtained from the patients’ parents.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hu J, Shi C, Li Z, et al. A cluster of cases of severe fever with thrombocytopenia syndrome bunyavirus infection in China, 1996: A retrospective serological study. PLoS Negl Trop Dis 2018;12:e0006603. [Crossref] [PubMed]
- Yu XJ, Liang MF, Zhang SY, et al. Fever with thrombocytopenia associated with a novel bunyavirus in China. N Engl J Med 2011;364:1523-32. [Crossref] [PubMed]
- You AG, Yang JH, Tang XY, et al. Risk factors of severe fever with thrombocytopenia syndrome (SFTS) infected by SFTSV Chinese Journal of Zoonoses 2015;31:704-8. [J].
- Ding F, Guan XH, Kang K, et al. Risk factors for bunyavirus-associated severe Fever with thrombocytopenia syndrome, china. PLoS Negl Trop Dis 2014;8:e3267. [Crossref] [PubMed]
- Hu JL, Li ZF, Wang XC, et al. Risk Factors for Bunyavirus-Associated Severe Fever with Thrombocytopenia Syndrome: A Community-Based Case-Control Study. PLoS One 2016;11:e0166611. [Crossref] [PubMed]
- Gong Z, Gu S, Zhang Y, et al. Probable aerosol transmission of severe fever with thrombocytopenia syndrome virus in southeastern China. Clin Microbiol Infect 2015;21:1115-20. [Crossref] [PubMed]
- Gai Z, Liang M, Zhang Y, et al. Person-to-person transmission of severe fever with thrombocytopenia syndrome bunyavirus through blood contact. Clin Infect Dis 2012;54:249-52. [Crossref] [PubMed]
- Bao CJ, Guo XL, Qi X, et al. A family cluster of infections by a newly recognized bunyavirus in eastern China, 2007: further evidence of person-to-person transmission. Clin Infect Dis 2011;53:1208-14. [Crossref] [PubMed]
- Chen H, Hu K, Zou J, et al. A cluster of cases of human-to-human transmission caused by severe fever with thrombocytopenia syndrome bunyavirus. Int J Infect Dis 2013;17:e206-8. [Crossref] [PubMed]
- Ding S, Niu G, Xu X, et al. Age is a critical risk factor for severe fever with thrombocytopenia syndrome. PLoS One 2014;9:e111736. [Crossref] [PubMed]
- Liu Q, He B, Huang SY, et al. Severe fever with thrombocytopenia syndrome, an emerging tick-borne zoonosis. Lancet Infect Dis 2014;14:763-72. [Crossref] [PubMed]
- Silvas JA, Aguilar PV. The Emergence of Severe Fever with Thrombocytopenia Syndrome Virus. Am J Trop Med Hyg 2017;97:992-6. [Crossref] [PubMed]
- Li Z, Hu J, Cui L, et al. Increased Prevalence of Severe Fever with Thrombocytopenia Syndrome in Eastern China Clustered with Multiple Genotypes and Reasserted Virus during 2010-2015. Sci Rep 2017;7:6503. [Crossref] [PubMed]
- Jiang XL, Zhang S, Jiang M, et al. A cluster of person-to-person transmission cases caused by SFTS virus in Penglai, China. Clin Microbiol Infect 2015;21:274-9. [Crossref] [PubMed]
- Ma T, Sun JM, Chen LF, et al. A pediatric case of severe fever with thrombocytopenia syndrome in Zhejiang Province, China. J Clin Virol 2015;72:85-7. [Crossref] [PubMed]
- Wang LY, Cui N, Lu QB, et al. Severe fever with thrombocytopenia syndrome in children: a case report. BMC Infect Dis 2014;14:366. [Crossref] [PubMed]
- Liu W, Lu QB, Cui N, et al. Case-fatality ratio and effectiveness of ribavirin therapy among hospitalized patients in china who had severe fever with thrombocytopenia syndrome. Clin Infect Dis 2013;57:1292-9. [Crossref] [PubMed]
- Cui F, Cao HX, Wang L, et al. Clinical and epidemiological study on severe fever with thrombocytopenia syndrome in Yiyuan County, Shandong Province, China. Am J Trop Med Hyg 2013;88:510-2. [Crossref] [PubMed]
Cite this article as: Zhang N, Li ZF, Ma T, Zhang Z, Li LX, Liu K, Wang XC, Liang SY, Bao CJ, Hu JL. A family cluster of pediatric cases of severe fever with thrombocytopenia syndrome following short-time exposure to a city park in China: case reports. J Public Health Emerg 2022;6:8.


