
Restaurant-associated foodborne illness outbreaks in the United States: an epidemiological assessment comparing outbreak occurrence and density before [2000–2019] and during [2020] the COVID-19 pandemic
Highlight box
Key findings
• Approximately 45% of foodborne illness outbreaks publicly available in the NORS database were associated with exposure at a restaurant.
• There was a statistically significant decrease in the number of outbreaks per year in 2020 compared to 20 years prior.
• No statistically significant difference was observed in foodborne outbreak density in restaurants between 2000 and 2019 compared to 2020 (i.e., the onset of the COVID-19 pandemic).
What is known and what is new?
• High rates of foodborne illness have persisted throughout history and prevention practices have plateaued. Findings from this study indicate that methods used by restaurants to enhance protection against COVID-19 transmission may not be the most effective in reducing foodborne illness outbreaks; however, by applying the chain of infection to the hierarchy of controls, both COVID-19 and foodborne illnesses can be better mitigated.
What is the implication, and what should change now?
• Approaches that incorporate food safety and COVID-19 prevention strategies should be utilized for optimized infection control in the food industry.
Introduction
Background
Foodborne illnesses remain an ongoing challenge in the United States (US) hospitality and tourism industry (1). The US observes an estimated 48 million cases of foodborne illnesses per year, equating to approximately one in six Americans, approximately 128,000 foodborne hospitalizations per year, and approximately 3,000 foodborne deaths per year (2). The Centers for Disease Control (CDC) highlights five pathogens that cause the most foodborne illnesses each year as norovirus, Salmonella (nontyphoidal), Clostridium perfringens, Campylobacter spp., and Staphylococcus aureus; five pathogens that cause the most foodborne hospitalizations as Salmonella (nontyphoidal), norovirus, Campylobacter spp., Toxoplasma gondii, and E. coli (STEC) O157; and five pathogens that cause the most foodborne deaths as Salmonella (nontyphoidal), Toxoplasma gondii, Listeria monocytogenes, norovirus, and Campylobacter spp. (2).
Hospitality establishments, such as restaurants, are required to adhere to foodborne illness guidelines and requirements, such as food temperature and sanitization practices, as established by the US Food and Drug Administration (FDA) and state and local health authorities (3,4). During the COVID-19 pandemic, in efforts to reduce the spread of SARS-CoV-2, the highly transmissible respiratory virus responsible for causing COVID-19, many hospitality establishments adapted behaviors and best practices to accommodate new FDA guidelines, including four main categories related to cleaning and disinfection, hand washing, social distancing, and opting for delivery services (4,5). The restaurant industry was one of the most impacted industries of the COVID-19 pandemic, reporting an approximate loss of $240 billion in revenue at the end of 2020 (6). In efforts to combat continuous loss and to create safe and healthy operations in dining establishments, restaurants adapted their offsite operations including contactless delivery and pick up options as well as their onsite operations including improving ventilation systems, adhering to mask mandates, physical distancing (including enhanced wayfinding and signage to maintain physical boundaries), minimizing shared objects, use of personal protection equipment, and contactless services and/or touchless facilities (6,7). These techniques can be grouped into the “servicescape” environment that were used to visually showcase a restaurant’s commitment to reducing the spread of COVID-19 and creating a clean, healthy, and safe environment for their patrons (6). As a result of these various risk mitigation and hazard control strategies, the dining experience drastically changed during the COVID-19 pandemic as restaurants attempted to increase protections against infection.
It is possible that the COVID-19 risk mitigation practices that collectively enhanced defenses against COVID-19 transmission in restaurants and food establishments may have also helped lead to a decline in enteric infections in the US. A 2020 Special Issue report of the International Journal of Environmental Research and Public Health notes that “despite decades of government and industry interventions”, food-borne illnesses remain “unexpectedly high in both developed and developing nations” (8). Despite widespread knowledge that foodborne diseases are preventable, it seems that there has been a plateau in the advancement of prevention practices (8). With the pandemic-related additions to food service safety in the form of COVID-19 infection control, there is a possible arena for increased prevention of foodborne illnesses. Recent studies have examined changes in foodborne illness outbreak occurrences and trends during the COVID-19 pandemic (approximately 2020 to 2022) (9-11). In Colorado, data on acute gastroenteritis (AGE) were examined for 2020 and compared to trends between 2017 and 2019 using electronic health record data from the Colorado Health Observation Regional Data Service (9). Researchers found a decrease of 52% in AGE in 2020 compared to the annual averages of 2017 through 2019 (9). Additionally, researchers observed that historical trends including seasonality and pediatric encounters were no longer evident in the data presented. In a nation-wide study using data from the Foodborne Diseases Active Surveillance Network (FoodNet) of the CDC’s Emerging Infections Program, researchers observed similar decreases: gastrointestinal illnesses caused by eight common enteric pathogens decreased 26% in 2020 compared to 2017 to 2019 (11). In the most recent update, researchers found an eight percent decrease in enteric illness reported in 2021 compared to the 2016 to 2018 average in FoodNet (10).
Rationale and knowledge gap
Previous studies did not examine specific reasons for these observed decreases in foodborne illness trends, such as determining whether they were related to pandemic restrictions, environmental adjustments, behavioral modifications (e.g., changes in those seeking medical care), or other potential factors (9-11). These limitations inhibit the ability to conclude whether control measures in COVID-19 risk mitigation contributed directly to the decrease in foodborne illness cases that were seen in 2020 compared to previous years. Therefore, it remains unclear whether the risk reduction strategies used for COVID-19 also assisted in decreasing foodborne-related illness outbreaks in restaurants. Further, the aforementioned studies did not assess statistical significance in these observed foodborne illness outbreak reductions prior to and during the COVID-19 pandemic and did not assess for changes in outbreak incidence resulting from exposure in a restaurant.
Objective
The aim of this study was to evaluate epidemiological trends in foodborne illness outbreaks associated with restaurant dining prior to and during the COVID-19 pandemic (defined as pre-2020 and 2020) in the US to understand whether COVID-19 risk mitigation strategies may have additionally assisted in decreasing the occurrence and density of foodborne enteric illness outbreaks. Specifically, this study assessed potential changes in occurrence and density of foodborne illness outbreaks during the first year of the COVID-19 pandemic (i.e., 2020) using publicly available epidemiological data from the CDC’s National Outbreak Reporting System (NORS). Further, the study explored societal level behavior changes related to restaurant dining during the COVID-19 pandemic. Based on these findings, recommendations for hazard control and risk mitigation strategies were provided which consider the use of the National Institute for Occupational Safety and Health (NIOSH) hierarchy of controls implemented in the chain of infection model to better inform Hazard Analysis and Critical Control Points (HACCP) Planning.
Methods
Data were obtained from the CDC’s NORS to evaluate trends in foodborne illness outbreaks associated with restaurant dining and other settings prior to and during the COVID-19 pandemic in the US; information from FoodNet was also utilized to inform data inclusion criteria. Only publicly available data on both platforms were utilized.
NORS and FoodNet
NORS is a web-based platform that collects and compiles information from state, local, and territorial public health agencies across the US to report foodborne and waterborne disease outbreaks, as well as enteric disease outbreaks transmitted via person-to-person, animal contact, environmental contamination, or other indeterminate means (12). For this analysis, only outbreak data where food was presumed or identified to be the vector were utilized. All data utilized in the present analysis are publicly available via the NORS Dashboard and additional data were not requested (13). Unlike NORS, which collects data from all 50 states and six US territories (Puerto Rico, Republic of Palau, Republic of the Marshall Islands, US Virgin Islands, Commonwealth of Northern Marina Islands, Guam), FoodNet only surveils seven states (Connecticut, Georgia, Maryland, Minnesota, New Mexico, Oregon, and Tennessee) and specific counties in three additional states (California, Colorado, and New York), which accounts for approximately 15% of the US population as a sentential surveillance system (14). FoodNet categorizes outbreaks by their causative pathogen and assesses the burden of foodborne illness by these pathogens, which are outlined below, as well as by type of food and outbreak setting. Although data were not utilized from FoodNet due to the limited information regarding the setting in which causative exposure resulting in foodborne illness occurred, the pathogens monitored in FoodNet were used to define the pathogens explored in this study as they are among some of the most common foodborne illness causing pathogens.
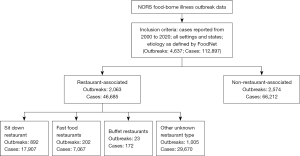
Publicly available data from NORS were utilized to evaluate enteric infection trends across the US. The inclusion criteria for foodborne illness outbreaks, defined as an event in which two or more individuals experience an illness from the ingestion of a common food in NORS can be found in Figure 1. Specifically, using the NORS dashboard, only outbreaks transmitted through food were included; the year in which the outbreak occurred was constrained to what was available in the database (i.e., 2000–2020); and data for suspected and confirmed cases in all states and settings were included. However, the NORS dataset was limited to only include outbreaks associated with the nine pathogens monitored by FoodNet: Campylobacter, Cryptosporidium, Cyclospora, Listeria, Salmonella, Shigella, Vibrio, Yersinia, and Escherichia coli (STEC) O157 and non-O157. The pathogens include seven bacteria and two parasites, all of which are commonly transmitted through food. While FoodNet does not monitor for all possible foodborne pathogens, the pathogens included are some of the most critical in causing foodborne illness, hospitalization, and/or death; as such, these were selected to approximate foodborne illness in the US.
Variables
As mentioned previously, each “foodborne illness outbreak” was defined as an event in which two or more individuals experienced an illness from a common food exposure, and a “case” represented each individual illness that occurred within that outbreak.
Foodborne illness setting groupings
Within the NORS database, the setting in which the exposure occurred is defined for each outbreak. Multiple settings can be reported for each outbreak, and as such, it is impossible to distinguish which setting was associated with which case in each outbreak. Therefore, each setting was considered as an individual event, which may result in an overestimate of events per setting. This can be observed in Figure 1 as each of the 46,685 cases may be categorized under more than one of the possible restaurant-specific settings. There were four possible restaurant-specific exposure settings: “Fast Foods”, “Buffet”, “Sit-Down”, or “Other or Unknown”. Outbreaks with any of these four restaurant-type exposure settings were classified as a “restaurant-associated foodborne illness outbreak” or “restaurant-associated outbreak”. Analyses were conducted by “restaurant-associated foodborne illness outbreaks” and by each of the four restaurant-specific exposure settings.
Foodborne illness etiology
Foodborne illness outbreaks were often categorized as being affiliated with more than one pathogen. As previously mentioned, the pathogens tracked in the FoodNet database were assessed in this analysis and each outbreak with more than one etiology was recategorized to be a single event for each etiology type. The defined pathogens were manually categorized by the species of the pathogens in which the etiology was defined.
Defining an event as prior to or during COVID-19
The cutoff date for considering an outbreak event as “prior to” as opposed to “during” the COVID-19 pandemic was defined as January 31, 2020, the date which the US Department of Health and Human Services declared the novel corona virus a public health emergency (15). The month of January in 2020 was excluded from all analyses comparing pre- and during-COVID-19 outbreaks and associated cases, as the public health emergency, which resulted in changes in restaurant dining practices, was not declared until the end of the month. Data were available for 20 years prior to the selected cutoff date (i.e., 2000 through 2019). Data for this entire 20-year period were considered “prior to” the COVID-19 pandemic and was used as the comparison years to “during” the COVID-19 pandemic (i.e., February through December 2020).
Summary statistics
The data were summarized by total number of outbreaks for each month and year, and by etiology and exposure setting. Specifically, the frequency of each exposure setting and nine etiologies for all outbreaks from 2000 to 2020 was determined. Additionally, the average number of cases per outbreak each year, the number of hospitalizations, and the number of deaths each year were summarized. Given the non-normality of the data, a Wilcoxon Rank Sum test was utilized to assess if there were statistically significant differences in the number of restaurant-associated foodborne illness cases per outbreak (i.e., density) when comparing the years prior to the COVID-19 pandemic (2000 to 2019) and the number of cases per outbreak observed in 2020. The number of hospitalizations and mortality associated with each outbreak was not assessed as the NORS database noted data gaps associated with the available data. Similarly, a one sample t-test was utilized to determine if there was a statistically significant decrease in the number of restaurant-associated foodborne illness outbreaks and cases prior to (2000 through 2019) and during 2020. Summary statistics and figures were developed using R (16).
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Results1
Foodborne illness outbreaks
From 2000 to 2020, 4,637 foodborne illness outbreaks were reported in the NORS database, corresponding to approximately 113,000 enteric illnesses caused by the predefined pathogens. Overall, the occurrence of foodborne illness outbreaks ranges from 132 to 340 outbreaks per year from 2000 through 2020 and the density ranged from 14.55 to 36.50 cases per outbreak during that time period. Across the 21 years evaluated, the year 2018 had the greatest number of outbreaks (n=340) and illnesses (n=8,677) (Table 1). Further, in 2002, 2003, 2006, 2008, and 2020 the average number of illnesses per outbreak was greater than 30 (Table 1).
Table 1
| Year | Average cases per outbreak | Outbreaks | Cases | Deaths* | Hospitalizations* | Restaurant-associated outbreaks [cases] |
|---|---|---|---|---|---|---|
| 2000 | 24.24 | 222 | 5,382 | 13 | 484 | 120 [3,153] |
| 2001 | 29.17 | 207 | 6,039 | 7 | 401 | 113 [2,792] |
| 2002 | 30.30 | 220 | 6,666 | 13 | 510 | 112 [3,858] |
| 2003 | 31.13 | 213 | 6,630 | 11 | 447 | 97 [2,410] |
| 2004 | 24.69 | 203 | 5,013 | 10 | 470 | 100 [2,338] |
| 2005 | 26.90 | 181 | 4,868 | 6 | 431 | 79 [2,627] |
| 2006 | 33.33 | 193 | 6,432 | 8 | 795 | 90 [2,143] |
| 2007 | 22.36 | 234 | 5,233 | 10 | 672 | 97 [2,521] |
| 2008 | 36.50 | 192 | 7,008 | 19 | 1,039 | 66 [1,370] |
| 2009 | 22.83 | 179 | 4,086 | 7 | 453 | 56 [765] |
| 2010 | 26.61 | 210 | 5,589 | 12 | 482 | 73 [3,662] |
| 2011 | 22.96 | 199 | 4,569 | 47 | 804 | 60 [1,466] |
| 2012 | 22.30 | 208 | 4,638 | 14 | 708 | 74 [1,338] |
| 2013 | 19.05 | 255 | 4,858 | 23 | 907 | 112 [1,905] |
| 2014 | 14.55 | 259 | 3,768 | 25 | 626 | 113 [1,437] |
| 2015 | 21.31 | 258 | 5,497 | 17 | 840 | 116 [2,170] |
| 2016 | 18.56 | 223 | 4,138 | 18 | 666 | 96 [1,358] |
| 2017 | 21.79 | 227 | 4,946 | 22 | 881 | 103 [1,356] |
| 2018 | 25.52 | 340 | 8,677 | 20 | 1,381 | 182 [3,944] |
| 2019 | 17.00 | 282 | 4,794 | 5 | 858 | 149 [2,234] |
| 2020 | 30.80 | 132 | 4,066 | 7 | 569 | 55 [1,838] |
*, CDC NORS Database notes data gaps for this information. CDC, Centers for Disease Control; NORS, National Outbreak Reporting System.
Restaurant-associated foodborne illness outbreaks
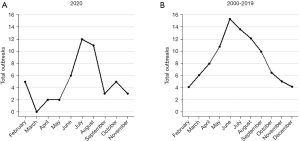
Nearly half (44.5%) of the outbreaks reported between 2000 and 2020 listed a restaurant-associated setting as one of the exposure settings, including: Food (drive up service or pay at counter), Buffet, Sit-Down Dining, and Other or Unknown restaurant type (Table 2). Additionally, over 20% of the outbreaks were associated with a private home residence (n=1,022) and the remaining exposure settings were reported at lower frequencies. Further, in 2018, there were more restaurant-associated outbreaks (n=182) and illnesses (n=3,944) than any other year (Table 1). Prior to the onset of COVID-19, from 2000 to 2019, there was a steady increase in cases from February until the total number of outbreaks per month peaked in June and steadily declined until December; however, during 2020, foodborne illness outbreaks dropped in March, April, and May (Figure 2). There were no restaurant-associated foodborne illness outbreaks reported in March of 2020 in the publicly available NORS dashboard (Figure 2).
Table 2
| Setting | Number of outbreaks, n (% frequency) |
|---|---|
| Banquet facility (food prepared and served on-site) | 60 (1.13) |
| Camp | 38 (0.71) |
| Caterer (food prepared off-site from where served) | 257 (4.83) |
| Child day care | 15 (0.28) |
| Fair, festival, other temporary or mobile services | 81 (1.52) |
| Farm/dairy | 56 (1.05) |
| Grocery store | 220 (4.13) |
| Hospital | 26 (0.49) |
| Hotel/motel | 2 (0.04) |
| Long-term care/nursing home/assisted living facility | 66 (1.24) |
| Office/indoor workplace | 29 (0.54) |
| Prison/jail | 81 (1.52) |
| Private home/residence | 1,022 (19.2) |
| Religious facility | 68 (1.28) |
| Restaurant—“fast-food” (drive up service or pay at counter)* | 202 (3.79) |
| Restaurant—Buffet* | 23 (0.43) |
| Restaurant—other or unknown type* | 1,005 (18.88) |
| Restaurant—sit-down dining* | 892 (16.75) |
| School/college/university | 68 (1.28) |
| Other | 478 (8.98) |
| Other healthcare facility | 1 (0.02) |
| Unknown | 634 (11.91) |
| Total | 5,324 (100.00) |
*, restaurant-associated foodborne illness outbreak.
Given the data’s nature, an outbreak may be associated with more than one exposure setting, so the number of illnesses within each outbreak associated with each exposure setting is not identifiable. Overall, 501 out of the 4,637 outbreaks assessed had more than one exposure setting. Specifically, 2,063 of the outbreaks reported in NORS between 2000 and 2020 had a restaurant listed as one exposure setting; however, only 1,782 outbreaks were solely associated with a restaurant and 281 outbreaks included one or more of the other predefined settings as a place of exposure (Table 2).
Etiology of the foodborne illness outbreaks
Across all years evaluated, Salmonella spp. accounted for approximately 60% of all foodborne illness outbreaks, regardless of exposure setting (Table 3). The next most common illness causing pathogens identified were Escherichia spp. (14.28%) and Campylobacter spp. (12.46%). Similar trends were observed for outbreaks associated with exposure at a restaurant: approximately 61%, 13%, and 10% of outbreaks were associated with Salmonella spp., Escherichia spp., and Campylobacter spp., respectively.
Table 3
| Pathogen genus | Frequency of outbreaks, n (% frequency) |
|---|---|
| Campylobacter | 578 (12.13) |
| Cryptosporidium | 44 (0.92) |
| Cyclospora | 128 (2.69) |
| Escherichia | 662 (13.89) |
| Listeria | 99 (2.08) |
| Salmonella | 2,803 (58.81) |
| Shigella | 178 (3.73) |
| Vibrio | 205 (4.30) |
| Yersinia | 16 (0.34) |
| Other | 53 (1.11) |
| Total | 4,766 (100.00) |
Similar to how exposure settings are defined in each outbreak, outbreaks may also be associated with more than one pathogen. Specifically, 248 of the 4,637 outbreaks had more than one pathogen listed as the possible etiology of the illnesses associated with the outbreak.
Comparison of restaurant-associated outbreaks prior to and during the COVID-19 pandemic
A statistically significant decrease was observed in the number of foodborne illness outbreaks (P<0.001; 95% CI: 84.31 to Inf) and cases (P=0.017; 95% CI: 1,809.17 to Inf) associated with a restaurant exposure between the years leading up the COVID-19 pandemic [2000–2019] and the onset year of the COVID-19 pandemic [2020]. Overall, there was a 49% decrease in outbreaks in 2020 (49.00 outbreaks) compared to the average number of outbreaks per year from 2000 to 2019 (95.55 outbreaks), but only a 21% decrease in the total average infections per year between the two time periods (2020: 1,698.00 illnesses; 2000–2019: 2,159.80 illnesses). In contrast, there was not a statistically significant difference in the density of the outbreaks (number of foodborne illnesses per outbreak) in 2020 when compared to years prior to the COVID-19 pandemic (2000 to 2019) (P=0.598, 95% CI: −2.000037 to 1.000068). Specifically, there was an average of 34.65 restaurant-associated illnesses per outbreak in 2020 and an average of 23.06 illnesses per outbreak between 2000 and 2019.
While it appears there were a greater number of illnesses per restaurant-associated outbreak observed in 2020 than nearly every other year since 2000, excluding 2002 and 2010 (Table 4), there was one single multistate Salmonella outbreak that occurred in June 2020 which resulted in 1,132 foodborne illness cases. If this single datapoint is removed as a potential outlier, the average number of restaurant-associated foodborne illness cases per outbreak is reduced to 11.8. However, even when this potential outlier is removed, there remains no statistically significant difference between the density of outbreaks prior to [2000–2019] and during the COVID-19 pandemic [2020] (P=0.439; 95% CI: −2.0000187 to 0.9999179).
Table 4
| Year | Average cases per outbreak | Outbreaks | Cases |
|---|---|---|---|
| 2000 | 27.13 | 115 | 3,120 |
| 2001 | 25.66 | 105 | 2,694 |
| 2002 | 35.19 | 105 | 3,695 |
| 2003 | 24.77 | 93 | 2,304 |
| 2004 | 24.22 | 95 | 2,301 |
| 2005 | 33.99 | 77 | 2,617 |
| 2006 | 23.68 | 82 | 1,942 |
| 2007 | 26.53 | 93 | 2,467 |
| 2008 | 22.11 | 61 | 1,349 |
| 2009 | 13.94 | 54 | 753 |
| 2010 | 52.09 | 70 | 3,646 |
| 2011 | 24.98 | 58 | 1,449 |
| 2012 | 13.26 | 65 | 862 |
| 2013 | 17.04 | 111 | 1,891 |
| 2014 | 12.65 | 110 | 1,392 |
| 2015 | 18.82 | 115 | 2,164 |
| 2016 | 15.01 | 88 | 1,321 |
| 2017 | 13.27 | 99 | 1,314 |
| 2018 | 21.72 | 173 | 3,758 |
| 2019 | 15.19 | 142 | 2,157 |
| 2020 | 34.65 | 49 | 1,698 |
Discussion
Key findings
The COVID-19 pandemic presented a variety of challenges and altered the way in which the US produces, processes, prepares, serves, and obtains food (17). Considering nine of the most common pathogens that cause foodborne illnesses, the present analysis found that approximately 45% of foodborne illness outbreaks are associated with restaurants in the US (Table 2). Further, this study found a significant difference in the number of foodborne illness outbreaks and cases observed from February to December of 2020 (i.e., during the COVID-19 pandemic) compared the 20 years prior, thus indicating an overall change in the occurrence of foodborne enteric illness outbreaks associated with restaurants. However, despite a reduction in the number of outbreaks observed in 2020 compared to previous years, there was no statistically significant difference in the number of cases per outbreak, suggesting that the density of disease outbreaks was not reduced by COVID-19 safety protocols and practices.
Explanations of findings and comparison with similar research
Although SARS-CoV-2 is not a foodborne pathogen, its viral spread has affected dining habits and food safety approaches during a time of increased infection control practices (18). Previous studies found a decrease in foodborne illnesses in 2020 compared to earlier years (9-11). Another study observed greater decreases in foodborne illness outbreaks in states with more stringent COVID-19 restrictions, particularly with pathogens associated with restaurant dining (19). Researchers also observed an overall decrease in restaurant-associated dining indicative of a societal-level behavioral change due to the pandemic restrictions (19).
Similarly, the findings of this study illustrate a reduction in the number of restaurant-associated foodborne illness outbreaks observed in 2020 compared to the 20 years prior. Due to limited resources from COVID-19 protocols and health agency reporting, foodborne illness outbreaks in 2020 were possibly reported at decreased rates (11). Further, the CDC indicates that foodborne illness outbreaks may be underreported to the CDC due to the voluntary nature of foodborne illness reporting (20). Changes in access and behavior during the pandemic may have also impacted the number of foodborne illnesses reported to the health departments (11,21). Additionally, given indoor dining restrictions and wide-reaching COVID-19 regulations, it is possible that a reduction in restaurant-associated foodborne illness outbreaks were observed because people were ordering from or dining at restaurants less than previous years. While anecdotal evidence suggests that observed decreases in foodborne illness outbreaks may be due to increased public health measures specific to COVID-19, no specific data could confirm these findings (22-25). Other factors, such as telecommuting during the COVID-19 pandemic, may have also been negatively associated with indoor dining or less individuals choosing to dine at a restaurant (26).
Between 2015 and 2019, foodborne illness outbreaks were reported in 46 states as well as Puerto Rico and Washington, DC. Conversely, foodborne illness outbreaks were only reported in 21 states in 2020. This decrease in states reporting foodborne illness outbreaks may be due in part to the aforementioned challenges faced by health departments as well as among individuals and communities around the country. However, despite that there were fewer foodborne illness outbreaks and total associated illnesses, the findings of this study represent that during the COVID-19 pandemic (in which there was a decreased restaurant activity and increased infection prevention strategies), the density of these foodborne illness outbreaks is not statistically significantly different from pre-COVID years (4,27,28). In sum, at each foodborne illness outbreak incident there were not fewer associated illnesses. Therefore, in establishing disease control or risk reduction relationships, it would be expected and desired that both the occurrence and the density of outbreaks be reduced.
This is consistent with the transmission pathways of common foodborne pathogens that are not routinely transmitted in the same way (e.g., aerosol or droplet pathways) as SARS-CoV-2 (except for viruses like norovirus). Notably, none of the pathogens monitored by FoodNet are viruses [e.g., Campylobacter, Cryptosporidium, Cyclospora, Listeria, Salmonella, Shigella, Vibrio, Yersinia, and Escherichia coli (STEC) O157 and non-O157]. As a result, the findings suggest that most of the common foodborne illnesses may not be mitigated or controlled by viral respiratory infection prevention practices as instituted during the COVID-19 pandemic.
Incorporating COVID-19 and food safety protocols
Many of the precautions taken during the COVID-19 pandemic focused on food pick-up, delivery, and indoor and outdoor dining protections to minimize the transmission of COVID-19, yet many were not specific to traditional food safety precautions or the mitigation of foodborne illnesses. While hand and surface hygiene are highly applicable to all disease spread and are considered important factors in controlling the spread of foodborne illnesses, some safety measures implemented during the COVID-19 pandemic and in restaurant-like settings (e.g., masking, social distancing, increased ventilation) may not be as effective in mitigating the spread of foodborne diseases, which may not be commonly spread by aerosol or droplet pathways (18,29-31).
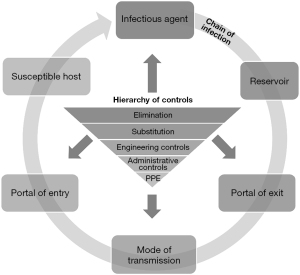
The primary goal of risk mitigation is to reduce the risk of adverse health effects by controlling exposure and proliferation to a particular hazard or multiple hazards, regardless of the population or potential routes of exposure. When controlling a potential hazard is complex (e.g., foodborne pathogens and SARS-CoV-2) with variable risk sources and transmission routes, implementing a combination of measures to create a multilayered and flexible risk mitigation approach becomes necessary. By implementing several risk mitigation measures simultaneously, overall transmission risk will be minimized (32). A comprehensive multilayered infection control plan can be created by applying three well-established frameworks: HACCP, the chain of infection, and the hierarchy of controls.
HACCP is an internationally recognized food safety management system commonly used by food safety professionals to proactively identify, control, and monitor biological, chemical, and physical hazards (5,33). To break the cycle of disease transmission, Zisook et al. [2020] argued for adapting the NIOSH hierarchy of controls framework for infection control and prevention and integrating it into the chain of infection model (32,34,35) (Figure 3). For restaurants, it would therefore be compelling that HACCP also incorporate specific aspects of the hierarchy of controls and chain of infection hybrid model for a more holistic approach to infection prevention (e.g., foodborne pathogens and SARS-CoV-2). As mentioned previously, in addition to common foodborne bacterial pathogens (e.g., E. coli, Salmonella spp., Campylobacter spp., Listeria spp.), risk of exposure to viral pathogens (e.g., noroviruses, rhinoviruses) at food service facilities have been, and will remain, a threat to restaurant dining venues. While HACCP planning has traditionally been used to address specific food safety practices and procedures within and among kitchen operations, it can also evolve to work with the infection control hybrid model to specifically prevent disease transmission influenced or originating from outside of kitchen operations (e.g., SARS-CoV-2). For example, specific critical control points addressing concerns related to self-service by patrons, gatherings near or around food areas, congregate dining locations, and exposed or unprotected foods in common dining areas could be identified and evaluated by the aforementioned hybrid model, while corrective actions can be taken, and controls continually monitored by HACCP’s seven principles. While these control measures are not novel, they can be optimized and tailored to provide robust controls that better address the unique and varying needs of different foodservice industries, particularly where variable risk sources for disease transmission are present. Understanding and instituting more holistic and multilayered disease control practices will only help restaurants effectively prepare for and respond to future outbreaks or pandemics.
Limitations
One benefit of the present analysis is that the data utilized is entirely publicly available and updated annually making the present analysis easily reproducible and replicable from year to year. Nonetheless, there are inherent limitations to the data provided by NORS. Primarily, collection of the data was solely reliant on data reporting by local and state health agencies. During times of public health crisis, such as pandemics, health departments are often strained for resources which could potentially lead to less frequent reporting of health issues that are not as critical to the current public health emergency (36). Additionally, the CDC states that publicly available data are not complete and additional data can be provided upon request. However, to ensure full data transparency, only publicly available data were utilized in this current study and used as a representative dataset to assess trends.
In addition, the CDC has identified 31 known pathogens that cause foodborne illness, nine of which are surveyed by FoodNet. Notably, there are several pathogens listed in CDC’s top five for foodborne illness, hospitalization, and/or death that are not monitored by FoodNet (e.g., norovirus, Toxoplasma Gondii, Clostridium perfringens, and Staphylococcus aureus). In limiting the outbreak data to pathogens monitored by FoodNet, the number of foodborne-related outbreaks may have been underestimated. Similarly, since FoodNet only conducts surveillance on the aforementioned bacterial and parasitic species, outbreaks related to viral pathogens (e.g., norovirus) may have changed this analysis and could be a future subject of research.
Additionally, given the available data, there was no way to control for the potential effects of reduced restaurant dining activity that may have occurred following the onset of the COVID-19 pandemic, potentially limiting the ability to conclude that COVID-19 risk mitigation strategies effected foodborne illness spread.
Lastly, it is not possible to identify that each of the illnesses within the “restaurant-associated” outbreaks, as defined by this analysis, are associated with an exposure that occurred at a restaurant. As mentioned previously, some of the outbreaks had multiple exposure settings listed with no definitive way to categorize each of the illnesses in that outbreak with a specific setting. Thus, for the purposes of this assessment, the number of restaurant-associated foodborne illness cases may have been overestimated. As dining trends and best practices regarding safety continue to evolve in the post-COVID-19 world, future research should examine data from additional years of NORS data to assess how outbreak trends change.
Conclusions
It is evident from this evaluation and similar studies, that there was a reduction in restaurant-associated foodborne illness outbreaks during the COVID-19 pandemic compared to earlier years; however, it is less clear if there was a reduction in the density of these outbreaks. These results suggest that COVID-19 risk mitigation strategies may not similarly enhance public protection against foodborne illnesses in restaurant settings. While the COVID-19 pandemic has enabled industry and society to consider alternative ways of performing typical day-to-day activities that limit disease risk, incorporation of safety protocols specific to COVID-19 may not be the most effective infection prevention strategies for foodborne illnesses. However, with thoughtful planning and key understanding of how the hierarchy of controls can be applied to the chain of infection model, both COVID-19 and foodborne illnesses can be better mitigated during the HACCP planning process for optimal disease prevention and overall public health protection.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Journal of Public Health and Emergency for the series “Global Environmental Health and COVID-19”. The article has undergone external peer review.
Peer Review File: Available at https://jphe.amegroups.com/article/view/10.21037/jphe-23-2/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jphe.amegroups.com/article/view/10.21037/jphe-23-2/coif). The series “Global Environmental Health and COVID-19” was commissioned by the editorial office without any funding or sponsorship. All the authors are currently, or were formerly (EB, MAC) employed by Stantec ChemRisk, a consulting firm that provides scientific advice to governmental bodies, corporations, law firms, and various scientific/professional organizations. Two of the authors (EB, MAC) are employed by Insight Exposure and Risk Sciences Group, a risk sciences consulting firm serving clients in public, private, and non-profit industries. No outside funding was received for planning or executing the study, analyzing the samples, interpreting the data, or writing this manuscript. MAC served as an unpaid Guest Editor of the series. The study design, execution, results, and interpretation are the sole responsibility of the authors, and the text was prepared and written exclusively by the authors. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
Because COVID-19 was not yet declared a public health emergency by the US Department of Health and Human Services in January 2020, for consistency and comparison purposes, the month of January was excluded from all years in the analyses.
References
- Akil L. Trends of Foodborne Diseases in Mississippi: Association with Racial and Economic Disparities. Diseases 2021;9:83. [Crossref] [PubMed]
- CDC. Burden of Foodborne Illness: Findings: Centers for Disease Control and Prevention (CDC); 2018 [updated November 5, 2018. Available online: https://www.cdc.gov/foodborneburden/2011-foodborne-estimates.html
- CDC. Four Steps to Food Safety: Clean, Separate, Cook, Chill: Centers for Disease Control and Prevention (CDC); 2022 [updated August 5, 2022. Available online: https://www.cdc.gov/foodsafety/keep-food-safe.html
- FDA. Best Practices for Retail Food Stores, Restaurants, and Food Pick-Up/Delivery Services During the COVID-19 Pandemic: U.S. Food and Drug Administration (FDA); 2020 [updated April 21, 2020. Available online: https://www.fda.gov/food/cfsan-constituent-updates/fda-issues-best-practices-safe-food-handling-and-employee-health-retail-food-settings-during-covid
- FDA. Retail & Food Service HACCP: U.S. Food and Drug Administration (FDA); 2022 [updated March 7, 2022. Available online: https://www.fda.gov/food/hazard-analysis-critical-control-point-haccp/retail-food-service-haccp
- Xu Y, Singh S, Olson ED, et al. Consumers’ perceived effectiveness of COVID-19 mitigation strategies in restaurants: What went well and what could we do better? Int J Hosp Manag 2022;103:103206. [Crossref] [PubMed]
- Chen H, Eyoun K. Do mindfulness and perceived organizational support work? Fear of COVID-19 on restaurant frontline employees’ job insecurity and emotional exhaustion. Int J Hosp Manag 2021;94:102850. [Crossref] [PubMed]
- Todd E. Food-Borne Disease Prevention and Risk Assessment. Int J Environ Res Public Health 2020;17:5129. [Crossref] [PubMed]
- Armistead I, Tran A, White AE, et al. Trends in Outpatient Medical-Care Seeking for Acute Gastroenteritis During the COVID-19 Pandemic, 2020. Foodborne Pathog Dis 2022;19:290-2. [Crossref] [PubMed]
- Collins JP, Shah HJ, Weller DL, et al. Preliminary Incidence and Trends of Infections Caused by Pathogens Transmitted Commonly Through Food - Foodborne Diseases Active Surveillance Network, 10 U.S. Sites, 2016-2021. MMWR Morb Mortal Wkly Rep 2022;71:1260-4. [Crossref] [PubMed]
- Ray LC, Collins JP, Griffin PM, et al. Decreased Incidence of Infections Caused by Pathogens Transmitted Commonly Through Food During the COVID-19 Pandemic - Foodborne Diseases Active Surveillance Network, 10 U.S. Sites, 2017-2020. MMWR Morb Mortal Wkly Rep 2021;70:1332-6. [Crossref] [PubMed]
- CDC. About NORS: Centers for Disease Control and Prevention (CDC); 2019 [updated November 4, 2019. Available online: https://www.cdc.gov/nors/about.html
- National Outbreak Reporting System (NORS) [Internet]. Center for Disease Control and Prevention (CDC) and National Center for Emerging and Zoonotic Infectious Diseases (NCEZID). 2022 [cited October 10, 2022]. Available online: https://wwwn.cdc.gov/norsdashboard/
- CDC. About FoodNet: Centers for Disease Control and Prevention (CDC); 2021 [updated September 23, 2021. Available online: https://www.cdc.gov/foodnet/about.html
- ASPR. Declarations of a Public Health Emergency: Administration for Strategic Preparedness and Response (ASPR); 2022 [updated December 22, 2022. Available online: https://aspr.hhs.gov/legal/PHE/Pages/default.aspx
- R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2022.
- Cable J, Jaykus LA, Hoelzer K, et al. The impact of COVID-19 on food systems, safety, and security-a symposium report. Ann N Y Acad Sci 2021;1484:3-8. [Crossref] [PubMed]
- Maragoni-Santos C, Serrano Pinheiro de Souza T, Matheus JRV, et al. COVID-19 pandemic sheds light on the importance of food safety practices: risks, global recommendations, and perspectives. Crit Rev Food Sci Nutr 2022;62:5569-81. [Crossref] [PubMed]
- Akil L, Ahmad HA. Socioeconomic impacts of COVID-19 pandemic on foodborne illnesses in the United States. Eur J Environ Public Health 2023;7:em0128. [Crossref] [PubMed]
- CDC. Using NORS Data: Centers for Disease Control and Prevention (CDC); 2019 [updated November 4, 2019. Available online: https://www.cdc.gov/nors/data/using-nors.html
- Pujolar G, Oliver-Anglès A, Vargas I, et al. Changes in Access to Health Services during the COVID-19 Pandemic: A Scoping Review. Int J Environ Res Public Health 2022;19:1749. [Crossref] [PubMed]
- Food Safety News. Decline in foodborne illnesses in England likely linked to COVID-19 restrictions 2022. Available online: https://www.foodsafetynews.com/2022/12/decline-in-foodborne-illnesses-in-england-likely-linked-to-covid-19-restrictions/
- Food Safety News. Researchers assess impact of COVID-19 measures on foodborne infections 2021 Available online: https://www.foodsafetynews.com/2021/01/researchers-assess-impact-of-covid-19-measures-on-foodborne-infections/
- Food Safety News. COVID-19 measures accompany decline of foodborne infections 2021. Available online: https://www.foodsafetynews.com/2021/02/covid-19-measures-accompany-decline-of-foodborne-infections/
- CDC. CDC Report on Foodborne Disease Trends Shows Marked Declines During COVID-19 Pandemic: Centers for Disease Control and Prevention (CDC); 2021. Available online: https://www.cdc.gov/foodsafety/newsletter/foodborne-disease-trends-decline.html
- Abebe GK, Charlebois S, Music J. Canadian consumers’ dining behaviors during the COVID-19 pandemic: Implications for channel decisions in the foodservice industry. Sustainability 2022;14:4893. [Crossref]
- Dube K, Nhamo G, Chikodzi D. COVID-19 cripples global restaurant and hospitality industry. Current Issues in Tourism 2021;24:1487-90. [Crossref]
- Yang Y, Liu H, Chen X. COVID-19 and restaurant demand: early effects of the pandemic and stay-at-home orders. International Journal of Contemporary Hospitality Management. 2020;32:3809-34. [Crossref]
- Bosch A, Gkogka E, Le Guyader FS, et al. Foodborne viruses: Detection, risk assessment, and control options in food processing. Int J Food Microbiol 2018;285:110-28. [Crossref] [PubMed]
- Lacombe A, Quintela I, Liao YT, et al. Food safety lessons learned from the COVID-19 pandemic. J Food Saf 2021;41:e12878. [Crossref] [PubMed]
- O’Shea H, Blacklaws BA, Collins PJ, et al. Viruses associated with foodborne infections. Reference Module in Life Sciences 2019. doi:
10.1016/B978-0-12-809633-8.90273-5 .10.1016/B978-0-12-809633-8.90273-5 - Cappello MA, Hernandez AM, Lauer D, et al. Risk mitigation and disease control challenges of SARS-CoV-2 multidirectional transmission at ski resorts. J Public Health Emerg 2022;6:14. [Crossref]
- Safe Food Alliance. The Essential Guide To HACCP: Save Food Alliance. Available online: https://safefoodalliance.com/food-safety-resources/haccp-overview/
- Zisook RE, Monnot A, Parker J, et al. Assessing and managing the risks of COVID-19 in the workplace: Applying industrial hygiene (IH)/occupational and environmental health and safety (OEHS) frameworks. Toxicol Ind Health 2020;36:607-18. [Crossref] [PubMed]
- National Institute for Occupational Safety and Health (NIOSH) (2015) Hierarchy of controls. (Accessed 3 September 2020). Available online: https://www.cdc.gov/niosh/topics/hierarchy/default.html
- Pagaoa M, Grey J, Torrone E, et al. Trends in Nationally Notifiable Sexually Transmitted Disease Case Reports During the US COVID-19 Pandemic, January to December 2020. Sex Transm Dis 2021;48:798-804. [Crossref] [PubMed]
Cite this article as: Stewart CK, Freid RD, Brewster RK, Sutherland EQ, Best EA, Cappello MA. Restaurant-associated foodborne illness outbreaks in the United States: an epidemiological assessment comparing outbreak occurrence and density before [2000–2019] and during [2020] the COVID-19 pandemic. J Public Health Emerg 2023;7:12.


