Ki-Bong Yoo1, Jin Ye Yeo2
1Division of Health Administration, College of Software and Digital Healthcare Convergence, Yonsei University, Wonju, Republic of Korea; 2JPHE Editorial Office, AME Publishing Company
Correspondence to: Jin Ye Yeo. JPHE Editorial Office, AME Publishing Company. Email: jphe@amegroups.com
This interview can be cited as: Yoo KB, Yeo JY. Meeting the Editorial Board Member of JPHE: Prof. Ki-Bong Yoo. J Public Health Emerg. 2024. https://jphe.amegroups.org/post/view/meeting-the-editorial-board-member-of-jphe-prof-ki-bong-yoo.
Expert introduction
Prof. Ki-Bong Yoo (Figure 1) is an associate professor at Division of Health Administration, Yonsei University Mirae Campus, and the leader of Public Health Big Data Center of Yonsei Institute of Health and Welfare. As a data scientist and domain analyst, he has empirically evaluated the effects of many health policies using national health insurance claim data and various other secondary data. He participated in creating a sample dataset of cancer patients and in developing a research project on recognizing medical utilization patterns. The current main research topic is to identify patterns in medical utilization and predict them.

Figure 1 Prof. Ki-Bong Yoo
Interview
JPHE: What drove you into the field of health policy evaluation?
Prof. Yoo: I think I was lucky. I studied computer science for my bachelor's degree and worked as a software engineer developing Electronic Medical Records (EMR) systems. Then, in 2012, I happened to start a graduate program in health policy. At that time, the big data paradigm emerged, requiring large-scale data processing capabilities. Since I was a software developer, I naturally began working to manage various public health data. I very much enjoyed observing actual phenomena and identifying effects, causes, and consequences using public health data. For this reason, I am still working in this field.
JPHE: Could you share your insight of the direction of public health using big data?
Prof. Yoo: With large-scale health insurance data and EMR data from medical institutions, we can conduct more personalized and customized policy evaluations. I think future research topics will be precision prevention medicine or precision policy, such as the perspectives of precision medicine. There are many considerations from the perspectives of equity and equality, but I believe the future direction is for both the populational and individual perspectives.
JPHE: In one of your talks, you proposed the use of existing accumulated data to enhance health management programs. Could you share how this method can enhance the cost-effectiveness of health management programs without compromising the comprehensiveness of data collected for evaluation?
Prof. Yoo: It would be possible if an ideal Personal Health Record (PHR) is introduced. No one has achieved this yet, but there has been work in progress. In Korea, each individual can download his/her complete medical utilization history and apply the model through the ‘My Data’ project (1). Currently, this project is in the pilot stage and is expected to be fully implemented by 2025. This is possible because of the National Health Insurance and single-payer system. If comprehensive data collection is difficult, it can still be helpful if individuals directly collect and input at least the diagnosis codes. According to the perspective of the disease network, which I am currently focusing on, this can somewhat help to predict future health risks.
JPHE: Recently, you are also researching on disease incidence and unrecognized patient detection using public health data. Could you share what are the current gaps that need to be addressed?
Prof. Yoo: Many disease incidences and unrecognized patient detection models mainly rely on examination information and image data. The core of my model, however, is to predict disease incidence and detect unrecognized patient based on health insurance claims data, using medical utilization and diagnosis codes. As medical utilization and diagnosis codes are derived from examination information or health status, they can be used for prediction models. However, the most frequently asked question for this model is "why." Although various artificial intelligence (AI) methodologies are being developed, they cannot provide an answer like the results of usual regression analysis. While technological development is necessary to address this, I also believe that we need to partially accept the black box nature of these models to use AI models for public health.
JPHE: Could you share any recent developments in your research plans, particularly regarding your intended research on disease networks at Northeastern University?
Prof. Yoo: I am developing a Korean-version disease network (Figure 2) based on recent cases from Denmark (2) and Austria (3). The disease network is created by deriving relationships between all ICD-10 diagnosis codes. I believe this network is valuable from the perspective of preventive medicine. Using this network can greatly assist in personalized disease prediction, selecting target diseases for health policies, understanding the impact of diseases, and identifying confounding variables. It is a very interesting area, and I believe disease network research will increase in the future. Please keep an eye on future developments in this area.
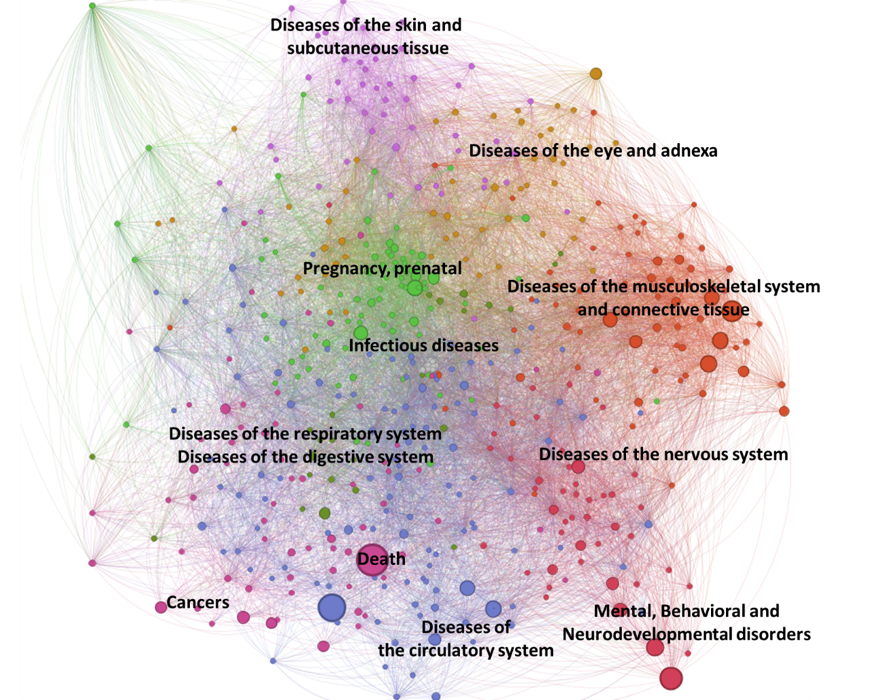
Figure 2 Preliminary disease network in Republic of Korea
JPHE: What are the current and emerging challenges of using big data to inform health care? What are some strategies that could be explored that can potentially overcome these challenges?
Prof. Yoo: Many people might mention security and such, but what I want to emphasize is integration. There are now a lot of big data, but they are not well linked due to security and authorization issues. However, comprehensive integration is necessary. Furthermore, a lot of research papers are being published, and a lot of evidence is being accumulated thanks to various big data. As research topics deepen, information is scattered. Therefore, it is important to integrate evidence from numerous studies. One of my long-term goals is to accumulate evidence based on disease networks. In an era overflowing with information, I believe it is necessary to build comprehensive evidence database at least once, like a kind of foundation model, and move on to the next generation of research.
JPHE: How has your experience been, and what are your expectation, as an Editorial Board Member of JPHE?
Prof. Yoo: I believe that JPHE has grown thanks to the excellent Editors-in-Chief and other outstanding members of the editorial board. Despite being a relatively new journal, I can feel that a lot of effort has gone into it. I hope that this journal will continue its current activities and become a foundational reference in public health for young researchers. I am thankful for this great opportunity.
Reference
Choi W, Chun JW, Lee SJ, et al. Development of a MyData platform based on the personal health record data sharing system in Korea. Applied Sciences. 2021;11(17):8208.
- Siggaard T, Reguant R, Jørgensen IF, et al. Disease trajectory browser for exploring temporal, population-wide disease progression patterns in 7.2 million Danish patients. Nat Commun. 2020;11(1):4952.
- Dervić E, Sorger J, Yang L, et al. Unraveling cradle-to-grave disease trajectories from multilayer comorbidity networks. npj Digit Med. 2024;7(1):1-12.
