
Ethical treatment of participants in public health research
Introduction
When judgment is recognized as a scientific tool, it is easier to see how science can be influenced by values. Values cannot—and should not—be separated from science. National Academy of Sciences, USA (1).
The abundant history of unethical research practices documented since Second World War (WWII) has proved, repeatedly, that the Hippocratic Oath can be broken in experimental settings (2). The Nuremberg Code, developed as a result of the Nuremberg Trial after the WWII, was the first document to set ethical standards for experiments involving humans. In 1964, the World Health Assembly met in Finland and drafted the first version of the Declaration of Helsinki (3), which, with its numerous updates, is recognized globally as one of the most authoritative guidelines on human research ethics. The Council for International Organizations of Medical Sciences (CIOMS) provides guidelines that indicate how the Declaration of Helsinki can be applied to biomedical research world-wide, especially in developing countries and vulnerable populations (4).
The Belmont Report describes three fundamental principles that form the basis of research ethics: respect, beneficence, and justice (5). Researchers embracing the three main ethical principles and their implementation, paralleled with research ethics committee approval and oversight, set the scene for responsible conduct of research. Research ethics is a mandatory component of all research involving humans. The question is “how” can one ensure that research is ethical?
Most journals require authors to affirm that the research was reviewed and approved by the relevant ethics authority, and, preferably, that it was conducted in compliance with international ethical standards. Although this statement is made in the final stage of the research—publication—it can only be made after the ground work has been done. In fact, ethical considerations should be inseparably integrated with any research study, from conception of the research idea, through protocol development, execution of the study, and dissemination of the results. To achieve this integration, the researcher needs to have a sound knowledge of research ethics, experience in its practical application, and ongoing evaluation of the ethical aspects of the project throughout.
In this article, I outline the principles of research ethics and explain how to incorporate ethical considerations into any public health research study. I also explain when ethics committee review is necessary and how researchers should go about obtaining an ethics review. Because of the differences between clinical biomedical research and public health research, wherever applicable, I comment specifically on the ethical aspects of public health research. I end with two examples that illustrate the difficulties in implementing ethical principles. Research misconduct, which has been covered extensively elsewhere, is beyond the scope of this article (6,7).
Respect
Informed consent
Respect for individuals involved in research means appreciating their autonomy—their independence and freedom to make a decision without external influences. They should be allowed to make an informed decision whether or not to participate in research based on both written and verbal information that has been provided to them through an informed consent process. In other words, individuals can only take part in research “voluntarily” (8). “Participation by individuals capable of giving informed consent as subjects in medical research must be voluntary.” (Declaration of Helsinki 2013-Paragraph 25) (9).
People whose ability to make decisions is compromised (such as children and individuals with impaired cognitive function) must have additional protections, in the form of surrogate consent by a legal guardian or legal representative. Surrogate consent to participate in research differs from the consent for receiving medical care. For example, it is usually sufficient for one or both parents to provide consent for their 10-year-old child to have surgery, whereas for research purposes, parental consent alone is not enough; the child would have to sign an “assent” form before participating in the study. Another example is that, in clinical care, in countries where the wife is not the legally authorized representative, she may be allowed to sign for her sick husband, whereas if that same patient was enrolled in a clinical trial, surrogate consent would need to be provided by the legally authorized representative, such as the son. Therefore, when obtaining surrogate consent, the researcher must know who the legally authorized representatives are in that country, otherwise the consent could be invalid.
Once a potential research participant gives informed consent, he or she can be enrolled in the study. Guidelines for the informed consent process for biomedical research are clear (10), although implementation can be challenging. The researcher must ensure that the consent process has been effective; first, by communicating with the potential participant using appropriate and understandable language, and second, by giving the participant an opportunity to ask questions and by assessing the participant’s understanding of the information that has been shared (11). Consent documents should be in the participant’s native language, and the informed consent process should be conducted by a researcher able to communicate with the participant in that language (12).
In public health research, two additional issues need to be considered: the circumstances under which exceptions to the rule of individual informed consent can be made and when community or group consent is necessary.
The Declaration of Helsinki makes exceptions for informed consent in certain situations. People who are physically or mentally incapable of giving consent (e.g., unconscious patients), may participate in research only if the physical or mental condition that prevents them from giving informed consent is what makes them eligible for the research. For example, research on the safety and effectiveness of a new product to prevent bedsores in bedridden individuals should exclude elderly persons with dementia because dementia is not a necessary inclusion criterion for the study. However, if the study is investigating a new drug for dementia, then the research would only be possible by recruiting people with dementia. To be able to recruit such patients, the researcher must seek informed consent from the legally authorized representative. If no such representative is available, and if the research cannot be delayed, the subject may be enrolled provided the “alternative recruitment procedures” including the measures for protecting safety, rights and well-being for such participants have been described in the protocol and approved by the ethics committee. Consent to remain in the research must be obtained as soon as possible from the subject or a legally authorized representative (10).
Consent may be waived for a study of an intervention affecting an entire community if: (I) research participants are at minimal risk; (II) it would not be possible to do the study by completing the consent process; and (III) the ethics committee has done a risk-benefit analysis and determined that waiving consent does not increase the risk of harm to the participants (see “Beneficence” section below) (13). When the research tests an intervention that involves an entire community, it can often be impractical to seek consent from each individual in that community. For example, in a study of the effects of water fluoridation on the incidence of dental carries, citizens essentially have to participate because fluoridated water is supplied to all households and water from another source is not readily available. Ethics committees have waived consent for such studies, in view of the difficulty of obtaining consent from each member of each household. To be successful and avoid criticism from the community (14), studies requesting a waiver of consent must at least involve the community through meetings, awareness campaigns, and open communication channels with researchers.
Another situation that may allow a public health study to be conducted without individual informed consent is an emergency, such as an epidemic or natural disaster. In such emergencies, almost always time is of the essence. Sometimes the time window during which the intervention must be given is narrow, precluding obtaining informed consent. Furthermore, this narrow time window may occur against a background of poverty, malnutrition, and compromised safety (15).
In some research involving communities, the consent of community leaders may be required (16). Consent is obtained through conversations with community leaders that develop mutual trust and respect. Researchers, particularly those not familiar with the community, should use this opportunity to learn about the customs and community practices that might affect the study. For example, even after community leaders have agreed to the study, in some cultures, the norm is for the head of the household (often the husband, father, or brother) to decide whether members of the family will be allowed to participate. In such cases, the informed consent process is a more complex, multi-stage progression, and simply applying standard Western consent processes will be inadequate (17). Although community leadership consent in most health research cannot replace individual consent, such consent may in some cases be sufficient, especially in research that is otherwise exempt (as described above).
For all research, whether the informed consent process is simple, more complex, or waived, ethics committee approval must be sought. The researchers cannot exempt their own research.
Basic requirements of informed consent documents
For informed consent to be valid, both the documents and the process need to be adequate. The documents at the very least should contain two sections: a Participant Information section and a Signature section. The Participant Information section should include the following information (10):
- A statement that the individual is invited to participate in a research study and that such participation is voluntary;
- A statement that declining to participate will not result in losing any rights or in any consequences;
- The purpose of the study;
- Why the individual has been chosen to participate;
- How many participants will be in the study;
- How long the study will last and details of study procedures, including what data will be collected and how;
- What the benefits of participating are and any potential risks participants will be exposed to;
- An explanation of who will have access to the individual’s data (confidentiality) and that the individual has the right to decline to participate or to withdraw from the research at any time, without penalty or prejudice;
- Contact information for the investigators (or their delegates) and the ethics committee, in case the participant has any concerns about the research.
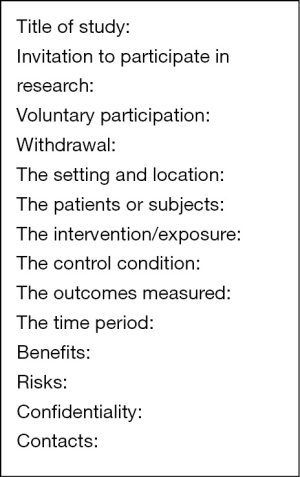
When preparing a consent form, the entries in Figure 1 can be useful sub-headings. These subheadings identify the minimum information that always needs to be included in a consent form. The language should be simple and easily understood by a layperson. Avoid technical terms unless they are necessary and are defined and explained in plain language. For example, instead of “hypertension”, use “high blood pressure”. However, “malignant hypertension” should be defined and explained: “malignant hypertension is extremely high blood pressure that develops rapidly and can damage internal organs, such as the kidneys, lungs, and heart. Malignant hypertension is a medical emergency and needs to be treated in a hospital, often in an intensive care unit”.
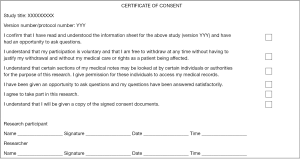
The Signature section has to have at the very least a place for participant’s name, signature and date, and the researcher’s name, signature and date (Figure 2). In special cases, for example, obtaining consent for an illiterate person or someone with dementia, the signature document must have provisions for the witness and or legally authorized representative to sign, as appropriate. Usually the Signature form will also have clauses confirming that participants have read the Information sheet, that the research has been explained to them, that they understand their participation is voluntary, that they can withdraw at any time, that they had an opportunity to ask questions, and that any of their concerns or queries have been addressed adequately.
Before the study, researchers should be trained on, or be familiar with, the different consent scenarios they may face, such as a participant who cannot read, a participant with a physical disability that prevents him or her from reading or signing the form, or a cognitively impaired participant or child who lacks legal status. Researchers should ensure that the consent process is conducted in a way that does not place any direct or indirect pressure on potential participants to consent. Examples of such influence include the power difference between a white-coated male doctor and a frail elderly woman, or peer pressure in a school setting.
Most journals require a statement saying that the study protocol was approved by the appropriate Institutional Review Board (IRB) and that written informed consent was obtained from adults and guardians and assent from children.
Privacy and confidentiality
Privacy means being protected from intrusion or observation without permission. In scientific investigations, researchers can only access information about a participant that the participant has agreed to divulge. Confidentiality is concerned with who has access to that information once it has been accessed by the researchers. The Declaration of Helsinki states: “Every precaution must be taken to protect the privacy of research subjects and the confidentiality of their personal information.” (Declaration of Helsinki 2013-Paragraph 24).
Maintaining confidentiality in research poses a number of challenges. Research usually involves a team of people, many of whom are likely to be exposed to private participant information. Researchers should have measures in place to protect such information from being accessed by anyone other than those authorized in the protocol and agreed to by the participant. Examples include “de-identifying” data by replacing names with a coded identifier, separating the data from the key to the coded identifiers, and storing data (both digital and print) securely by allowing only limited and authorized access. Nevertheless, breaches of confidentiality caused by human error or technical failure are always a potential risk. Damage from disclosure of confidential information can occur even when data are de-identified, particularly in research in small populations or communities where the participants can nevertheless be identified through deduction (18).
Another area where maintaining confidentiality is challenging is in qualitative research that involves participants in a group, such as focus groups. In such studies, where participants sit in small groups to discuss a topic, each participant’s information is exposed to the rest of the individuals in the group. Thus, participants should be told not to disclose their own information or that of other participants to people outside the group to avoid a direct or indirect breach of confidentiality (19).
Researchers should address confidentiality in the ethical considerations section of the study protocol. They should detail how and where data will be stored, who will have access to it, how long it will be stored, how it will be destroyed, and how the findings from the study will be disseminated. Safeguards to minimize risk of breach of confidentiality should be explained. When disseminating the results, through conferences or publication, data should be pooled and presented such that individual participants are not identified. Qualitative data should not be linked with individuals in a way that risks their identity. For example, the identity of this woman in a small rural village could be determined from her unedited quote: “I was forced to get married at the age of 14 and was instructed that I had to make sure that I meet all my husband’s needs and make sure he is happy. That was hard because he was 20 years older than me, had another wife, and 2 teenage daughters, all living with me.” Care should be taken to avoid stigmatizing or discriminating against individuals or groups as a result of information or findings shared in the study.
Beneficence
The second research ethics principle is beneficence, and it is coupled with non-maleficence. This principle is concerned with maximizing benefits and minimizing harm to research participants. Some early scientists believed that there should be no boundaries in the quest to further knowledge. In 1895, a prominent Chemist at the University of Chicago wrote, “A human life is nothing compared to a new fact in science. The aim of science is the advancement of human knowledge, at any sacrifice of human life” (20). Such attitudes, which were widespread in the United States until the middle of the twentieth century, led to the abuse of human subjects in the name of scientific research. Ethical guidelines changed this paradigm, so that now the welfare of the research subjects is always a priority. “In medical research on human subjects, considerations related to the well-being of the human subject should take precedence over the interests of science and society.” (Article 8, Declaration of Helsinki, 2001) (3).
To expand on this principle, each research study should undergo a risk-benefit analysis, which involves weighing any benefits (to the research participant or society) against potential risks. Benefits refer to all participants in a research study, not just to some. In a randomized controlled trial comparing two drugs for example, the research is only ethical if there is “clinical equipoise”, which means there is uncertainty about which drug is better; that there is no consensus in the medical community that favors one drug over the other (21). Risk encompasses all types of potential harm that could affect the research participant, either during or after the study. Physical harm, psychological harm, emotional harm, social harm, financial harm, reputational harm, and incrimination should all be considered, and risk mitigation measures should be incorporated in the design of the study. In some studies, where risk is considered minimal, meaning the probability and magnitude of harm or discomfort is no more than what the participant would normally encounter in daily life, a waiver of consent may be requested. A common example of research qualifying for exception to consent is a study involving a retrospective review of protected health information. However, if the information that needs to be accessed is personally sensitive, then even in the absence of direct contact with the participant, consent would be necessary.
For example, in a study comparing a new analgesic drug with a standard drug, patients whose pain is not controlled with either drug should be able to receive rescue medication that does not interact with the study drugs and known to be effective in relieving pain. Another example is a study of post-traumatic stress disorder in women who have suffered physical abuse. Participants in such a study may go through emotional distress while recalling or discussing their experiences, and their symptoms may even worsen after the study. For such a study, interviewers should be trained to recognize verbal and non-verbal cues of emotional distress and know how to deal with it. “Safety scripts” have been used as an additional protective measure, whereby the interviewer switches from the interview questions to an alternative script if the participant makes comments alluding to a serious problem, such as mentioning suicide (22,23). When necessary, options of immediate or subsequent follow up with a clinical psychologist or psychiatrist should be available (22).
Risk assessment involves considering not only the presence or absence of harm but also the severity of that harm, the likelihood of it occurring, and the extent of harm (i.e., will it affect only the participants, other individuals, or communities).
Public health research, as opposed to other types of health research, has additional considerations in risk assessment. In public health research, an important question to ask is “Who is the participant?” Is it an individual, a group, or a community? Or is it a combination? In research where the participant is a community, to what extent can individual rights and well-being be compromised for the greater benefit of the community? Examples of this are research projects with interventions that limit individuals’ freedom, such as no-smoking zones and compulsory use of seat belts.
A basic pre-requisite of beneficence is the scientific validity of the study. The research should be done according to sound methodology suited to the aims and objectives of the study. Research done with flawed methodology is unethical because it wastes resources, subjects the participants to procedures that are unlikely to be fruitful, and at the end could produce misleading results. This idea is clearly addressed in the Declaration of Helsinki: “Medical research involving human subjects must conform to generally accepted scientific principles, be based on a thorough knowledge of the scientific literature, other relevant sources of information, and on adequate laboratory and, where appropriate, animal experimentation.” (Declaration of Helsinki, 2013-Paragraph 21) (9). A scientifically valid study has several requirements, such as an appropriate study design, an adequate sample size determined by a power calculation to avoid a false negative result (Type 2 error), a duration long enough to observe an effect if there is one, outcome measures suitable for answering the research question, and measuring tools that are validated and reliable. The challenge with public health research is that it uses a wide variety of study designs and research methodologies, not all of which are the standard parallel-group comparisons typically used in clinical trials and other health research. For example, a policy or nationwide intervention, such as speed restrictions or mandatory helmet laws, cannot be tested with a parallel-group design.
The scientific aspects of the research should be reviewed by a scientific committee (if it exists), before ethics review. Alternatively, the ethics committee should conduct both a scientific and ethical review. Ethics committees should be able to conduct a rigorous review of the research proposals they receive, either with their existing members, or with the help of external reviewers in areas where different expertise is needed.
Justice
The principle of justice in research is about fair distribution of burdens and potential benefits of participation in research. The health of all members of a community or population is equally important, and all those who are eligible should have an opportunity to take part in research without discrimination. “Groups that are underrepresented in medical research should be provided appropriate access to participation in research.” (Declaration of Helsinki, 2013-Paragraph 13) (9). This provision, however, does not necessarily mean equal involvement of everyone in research, because the needs of certain sub-populations may differ from one another. Equity should be a key consideration, with sub-populations with the greatest health needs receiving priority (24).
Applying the principle of justice can be challenging. For example, in a population with health inequity, people who have access to certain facilities may be more likely to be considered for and to enroll in research, whereas the more disadvantaged continue to be marginalized. Another example is research in an identifiable community or ethnic group, where approval must go through the community leader. How does the leader influence the progress of the study? For instance, does the leader decide who gets recruited and who doesn’t? Does the leader have the authority to stop certain individuals from taking part? A third example is research in emergency situations, such as an earthquake. When medical supplies are low, and research is done to better understand how to improve health services in such situations, deciding who is recruited (and therefore who may get the better treatment) can be difficult.
The function of the research ethics committee
A Research ethics committee, otherwise known as an ethics review board, an IRB, an independent ethics committee, has been defined as a “group of individuals who undertake the ethical review of research protocols involving humans, applying agreed ethical principles” (25).
Research involving human subjects must be reviewed and approved by a research ethics committee before the research is begun. The Declaration of Helsinki clearly states that “The research protocol must be submitted for consideration, comment, guidance and approval to the concerned research ethics committee before the study begins.” (Declaration of Helsinki, 2013-Paragraph 23) (9).
Whether a certain project constitutes research is sometimes unclear. Research is “a systematic investigation (i.e., the gathering and analysis of information) designed to develop or contribute to generalizable knowledge” (26). Some interventions introduced as quality improvement and public health interventions can fall in a grey area that doesn’t quite fit the definition of research, particularly if there was no intention at the beginning to publish the results. In most cases, these “evaluative” projects share similar ethical issues with formal research (27). Health professionals should never decide on their own that a certain project is not research. The ethics committee should determine whether a given project requires review and approval.
Ethics committee approval cannot be obtained retrospectively “If a study has not been granted ethics committee approval prior to commencing, retrospective ethics approval usually cannot be obtained and it may not be possible to consider the manuscript for peer review. The decision on whether to proceed to peer review in such cases is at the Editor’s discretion” (28). Even if the study has no ethical issues of concern, the researcher cannot get clearance from the ethics committee after he has started the study. Furthermore, engaging in research before written approval from the ethics committee is considered to be a violation of the guidelines (9).
Putting it all together
Responsible conduct of research is not just knowing the three research ethics principles or published guidelines. It is about putting everything that has been discussed so far together in real life situations. I illustrate this point with two examples of public health research and discuss some of the ethical issues involved.
Research in emergency situations
CIOMS’s 2016 guidelines deal specifically with research in emergency and disaster situations (CIOMS guidelines, 2016—Guideline 20) (4). To develop improved disaster responses, research is considered to be an important and integral part of the disaster response. For example, between 2013 and 2016, West Africa experienced its worst Ebola virus epidemic, with mortality rates ranging from 40% to 100%. New prevention and treatment efforts had to be evaluated. Usually, new treatments can only be approved for further human research after sufficient safety and efficacy data have been collected, because with the lack of background data comes the increased risk of harm. However, for those affected, the experimental product was the only treatment, the only other option being the poor prognosis of a fatal disease. The seriousness of the situation and the urgent need for treatment skewed the risk-benefit analysis in favor of testing, although the supporting data were much less than what would be required in clinical trials. Accordingly, contrary to standard ethical guidelines, interventions that have not been approved for marketing by authorities such as the US Food and Drug Administration or the European Medicines Evaluation Agency, have been allowed in several research studies (29).
Informed consent and confidentiality are the cornerstones of the principle of respect. During an infectious disease epidemic, the informed consent process can be compromised in several ways. Qualified research staff who would otherwise be responsible for managing the informed consent process could be fully engaged in caring for individuals affected by the disease. In many cases, the vaccine must be delivered early to be effective, which means that taking a patient through a consent process would result in delaying treatment. During a disaster, resources normally available for research (office space and other research facilities) are often used for purposes other than research, and the resulting collapse of the research infrastructure may well impact some of the ethical aspects.
Furthermore, in such situations, health officials would be screening individuals known or suspected to be affected by the disease and would thereby be exposing themselves to the danger of contracting the disease.
Data are likely to be shared with local and international authorities, to determine the extent of disease outbreak, to understand the nature of spread of the virus, and to assess the effectiveness of new treatments. As such, in emergencies such as the Ebola outbreak, there may be an over-riding obligation to breach confidentiality by sharing data with stakeholders charged with reducing the suffering associated with the disease. In a review of 15 studies on Ebola virus, 7 did not have sufficient information regarding protection of participants’ privacy and confidentiality (30). In cases where necessary information is not mentioned in the publication, the authors cannot be given the benefit of the doubt. A generic statement about ethics committee review and approval might lead readers, at best, to infer that all ethical issues have been addressed.
One of the most difficult principles to implement during a disease outbreak is justice. Against a background of reduced health-care resources, shortage of staff, and limited supplies of a vaccine, what is the fairest way of deciding who is recruited to receive the vaccine? Given that health professionals, both caregivers and researchers, have maximum exposure to the virus, should they too receive the vaccine? In view of the limited supply, should they get priority? These questions have no simple answers; however, the criteria regarding recruitment should be clearly described in the protocol, reviewed and approved by the ethics committee, and adhered to by the researchers throughout the study.
Research with ethnic groups or small communities
Research with small, tight-knit populations, such as an indigenous community, has unique challenges. These challenges are illustrated in a qualitative study of spousal violence against Bedouin women. Bedouins are desert dwellers who live in tribes. In contrast to the Western focus on individual autonomy, in the Bedouin culture, the identity is that of the family, the extended family, and the tribe. A strong social hierarchy is marked by the dominance of males over females and older over younger (31).
What are the challenges with applying the principle of respect to such a study? Valid informed consent is central to conducting ethical research. That is, whether to participate in the research should be a voluntary decision made with no undue influence on any part. Investigating such a topic as sensitive as spousal abuse in a closed community carries a high risk of imposed refusal to participate (women whose husbands don’t want to be exposed) and forced participation (woman who have been pushed into the study to project a fake cover up of their abuse).
Ensuring confidentiality in such as study would be difficult, considering the small size and close-knit nature of the community. Sometimes, the woman is not allowed to go through the interview by herself and has to be accompanied by a “trusted other”, such as a sister-in-law or mother-in-law. In cases where the interview will be conducted in the presence of a relative, the researcher needs to develop strategies to ensure safety of the participants without compromising the validity of the results (32) (personal communication with Dr. Hala Hammad, Former Director of Child Safety Program, Jordan River Foundation, Amman, Jordan. September 2017).
What are the main issues in the risk benefit analysis of such a study? Findings from this study might assist government authorities and human rights activists to develop interventions that would help such women (33). However, this study could violate the community’s notions of privacy and infringe on their cultural traditions, in which a husband’s aggression towards his wife is accepted as normal or permitted behavior by both men and women. If domestic violence is a norm in the culture (34), many members of the community may see no point in exploring it through research. Importantly, the information that emerges from the study is likely to put the women at risk of further harm, as well as expose the behaviors of the spouse, which may be incriminating and have legal consequences.
Conclusions
❖ Ethical considerations should be an integral part of the research process from the initial planning stage, throughout the execution, and to the dissemination of results. Ethical aspects of research are as important as scientific aspects. The welfare of participants, whether individuals or communities, must always be respected. The rights, privacy, and safety of these participants take priority over other factors, which means that the validity of the research and its methods also fall under the umbrella of ethics.
❖ Several international guidelines present minimum standards and in each country, local laws, regulations, and customs must be viewed in parallel with (and not instead of) the international guidelines.
❖ Ethics in research is far from straightforward. Certain standards may be impossible to apply when immediate action is necessary to protect public health. In contrast, culturally sensitive issues may require more stringent safeguards in deference to the particular perspective of the research participants.
❖ Ethics requires a thorough understanding of the delicate balance between potential progress and potential harm, which is why it must underpin all research.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the the Guest Editor (Thomas A. Lang) for the series “Publication and Public Health” published in Journal of Public Health and Emergency. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jphe.2017.12.04). The series “Publication and Public Health” was commissioned by the editorial office without any funding or sponsorship. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- National Academy of Sciences, National Academy of Engineering, and Institute of Medicine. On Being a Scientist: A Guide to Responsible Conduct in Research: Third Edition. Washington, DC: The National Academies Press, 2009.
- Rice TW. The historical, ethical, and legal background of human-subjects research. Respir Care 2008;53:1325-9. [PubMed]
- Declaration of Helsinki (2001). Available online: http://www.who.int/bulletin/archives/79%284%29373.pdf. Accessed November 1, 2017.
- Council for Medical Research Involving Human Subjects. International Ethical Guidelines for Health Research Involving Humans. Available online: https://cioms.ch/wp-content/uploads/2017/01/WEB-CIOMS-EthicalGuidelines.pdf. Accessed November 1, 2017.
- The National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. The Belmont Report. Ethical Principles and Guidelines for the Protection of Human Subjects of Research. 1979. Available online: https://www.hhs.gov/ohrp/regulations-and-policy/belmont-report/index.html. Accessed November 1, 2017.
- Deshmukh MA, Dodamani AS, Khairnar MR, et al. Research misconduct: A neglected plague. Indian J Public Health 2017;61:33-6. [Crossref] [PubMed]
- Marusic A, Wager E, Utrobicic A, et al. Interventions to prevent misconduct and promote integrity in research and publication. Cochrane Database Syst Rev 2016;4:MR000038 [PubMed]
- Nijhawan LP, Janodia MD, Muddukrishna BS, et al. Informed consent: issues and challenges. J Adv Pharm Technol Res 2013;4:134-40. [Crossref] [PubMed]
- Declaration of Helsinki 2013. Available online: https://www.wma.net/wp-content/uploads/2016/11/DoH-Oct2013-JAMA.pdf. Accessed November 1, 2017.
- ICH Harmonised Guideline. Integrated Addendum to ICH E6(R1): Guideline for Good Clinical Practice, 2016. Available online: http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E6/E6_R2__Step_4_2016_1109.pdf. Accessed November 1, 2017.
- Kadam RA. Informed consent process: A step further towards making it meaningful! Perspect Clin Res 2017;8:107-12. [PubMed]
- Tekola F, Bull SJ, Farsides B, et al. Tailoring consent to context: designing an appropriate consent process for a biomedical study in a low income setting. PLoS Negl Trop Dis 2009;3:e482 [Crossref] [PubMed]
- Coughlin SS. Ethical Issues in Epidemiologic Research and Public Health Practice. Emerg Themes Epidemiol 2006;3:16. [Crossref] [PubMed]
- Barne-Rose R. Compulsory water fluoridation: justifiable public health benefit or human experimental research without informed consent? Wm & Mary Envtl L & Pol'y Rev 2014;39:201-41.
- Macklin R, Cowan E. Conducting research in disease outbreaks. PLoS Negl Trop Dis 2009;3:e335 [Crossref] [PubMed]
- World Health Organization Research Ethics Review Committee. The process of obtaining informed consent. Available online: http://www.who.int/rpc/research_ethics/Process_seeking_IF_printing.pdf. Accessed November 1, 2017.
- Upvall M, Hashwani S. Negotiating the informed-consent process in developing countries: a comparison of Swaziland and Pakistan. Int Nurs Rev 2001;48:188-92. [Crossref] [PubMed]
- Kaiser K. Protecting respondent confidentiality in qualitative research. Qual Health Res 2009;19:1632. [Crossref] [PubMed]
- Helgesson G. Informants a potential threat to confidentiality in small studies. Med Health Care Philos 2015;18:149-52. [Crossref] [PubMed]
- Dittrich L. Patient H.M.: A Story of Memory, Madness, and Family Secrets. New York: Penguin Random House LLC, 2017.
- Freedman B. Equipoise and the ethics of clinical research. N Engl J Med 1987;317:141-5. [Crossref] [PubMed]
- Labbot S, Johnson T, Feeny N, et al. Evaluating and addressing emotional risks in survey research. Survey Practice 2016. Available online: http://www.surveypractice.org/index.php/SurveyPractice/article/view/320. Date accessed: 23 Oct 2017.
- Draucker CB, Martsolf DS, Poole C. Developing distress protocols for research on sensitive topics. Arch Psychiatr Nurs 2009;23:343-50. [Crossref] [PubMed]
- Östlin P, Schrecker T, Sadana R, et al. Priorities for research on equity and health: towards an equity-focused health research agenda. PLoS Med 2011;8:e1001115 [Crossref] [PubMed]
- World Health Organizations. Research Ethics Committees. Basic Concepts for Capacity Building. Available online: http://www.who.int/ethics/Ethics_basic_concepts_ENG.pdf. Accessed October 23, 2016.
- Code of Federal Regulations. Definitions. Available online: https://www.hhs.gov/ohrp/regulations-and-policy/regulations/45-cfr-46/index.html#46.102. Accessed October 24 2017.
- Willison DJ, Ondrusek N, Dawson A, et al. What makes public health studies ethical? Dissolving the boundary between research and practice. BMC Med Ethics 2014;15:61. [Crossref] [PubMed]
- BMC Editorial Policies. Available online: https://www.biomedcentral.com/getpublished/editorial-policies#ethics+and+consent. Accessed November 1 2017.
- Alirol E, Kuesel AC, Guraib MM, et al. Ethics review of studies during public health emergencies—the experience of the WHO ethics review committee during the Ebola virus disease epidemic. BMC Med Ethics 2017;18:43. [Crossref] [PubMed]
- Richardson T, Johnston AM, Draper H. A systematic review of Ebola treatment trials to assess the extent to which they adhere to ethical guidelines. PLoS One 2017;12:e0168975 [Crossref] [PubMed]
- Al Krenawi A. 2002. The Struggle of Bedouin-Arab Women in a Transitional Society. Available online: https://escholarship.org/content/qt5fd390b0/qt5fd390b0.pdf. Accessed November 1 2017.
- Voltelen B, Konradsen H, Østergaard B. Ethical considerations when conducting joint interviews with close relatives or family: an integrative review. Scand J Caring Sci 2017; [Epub ahead of print]. [Crossref] [PubMed]
- Taft A, Colombini M. Healthcare system responses to intimate partner violence in low and middle-income countries: evidence is growing and the challenges become clearer. BMC Med 2017;15:127. [Crossref] [PubMed]
- Okour AM, Badarneh R. Spousal violence against pregnant women from a Bedouin community in Jordan. J Womens Health (Larchmt) 2011;20:1853-59. [Crossref] [PubMed]
Cite this article as: Al Tajir GK. Ethical treatment of participants in public health research. J Public Health Emerg 2018;2:2.


